MS Thesis Research Paper
Title
COMPARISON OF SURFACE TOPOGRAPHY AND X-RAY VALUES DURING IDIOPATHIC SCOLIOSIS TREATMENT USING THE CHÊNEAU BRACE
(THE CHÊNEAU BRACE SYSTEM)
Grant I. Wood
Institute for Health School of Health Care Professions
University of Salford, Salford, UK
Submitted in fulfillment of the Requirements of the Degree of Master of Science
April 2003
Abstract
An experiment was conducted to compare idiopathic scoliosis before Chêneau brace treatment with after treatment and determine if any significant changes in topography values (lateral deviation, rotation and trunk length) were present; and also reductions in Cobb and torsion angles. The subjects were 23 children diagnosed with progressive idiopathic scoliosis and/or presented a Cobb angle greater than 30 degrees, who were fitted and treated with the Chêneau brace during 4 years. The subjects’ surface topography was measured before and after treatment using the Formetric system, and the X-ray angles were measured using the Cobb and torsion angles. It was predicted that those who wore the Chêneau brace would report a reduction in Cobb and torsion angles as well as topography values compared with before the start of treatment. Significant differences were found in the topography values, also significant differences were found in the reduction of Cobb and torsion angles after wearing the Chêneau brace. Perhaps the most reasonable explanations for these findings are concerned with the effect of the three-dimensional design of the Chêneau brace. The strategically placed pressure points with the large expansion rooms provide space for correction of many aspects of the deformity. Since the incidence of progression of these subjects was high if untreated, the results were favourable.
Brace Studies
3.3 ORTHOTIC TREATMENT
3.3.1 BRACE TREATMENT FOR IDIOPATHIC SCOLIOSIS Charter 3, section 3.3.1 Literature review of scoliosis bracing, Master degree by thesis, Wood, 2003.
I) TLSO BOSTON BRACE STUDIES
Willers et al., (1993) presented the long-term effect of TLSO Boston brace treatment of the Cobb angle, vertebral rotation, rib hump and translation of the apical vertebra, in idiopathic scoliosis. Computed tomography measurements were completed before the start of treatment with the TLSO Boston brace and subsequently after bracing during an 8.5 years mean follow-up in 25 patients with idiopathic scoliosis. At follow-up, the pre-treatment Cobb angle, vertebral rotation, rib hump and the translation were not significantly decreased. As a result, this study demonstrated that the TLSO Boston brace does not improve, however prevents progression of the Cobb angle, vertebral rotation, rib hump and translation in idiopathic scoliosis. Willers et al., (1993) claimed that the reduction of the sagittal diameter was noteworthy and may be of importance for cosmesis and pulmonary function.Katz et al., (1997) presented a study of 319 patients with adolescent idiopathic scoliosis treated with either the TLSO Boston brace or a Charleston bending brace. The results found that the TLSO Boston brace is more effective than the Charleston bending brace, both in preventing lateral curve progression and in avoiding the need for surgery. These finding were most notable for patients with curves of 36 to 45 degrees Cobb angle in whom 83% of those treated with a Charleston bending brace had curve progression of more than 5 degrees, compared with 43% of those treated with the TLSO Boston brace. As a result, Katz et al., (1997) recommend the TLSO Boston brace and that the Charleston bending brace should be considered only in the treatment of smaller single thoracolumbar or single lumbar curves.Goldberg et al., (1993) reported two groups of 32 girls with adolescent idiopathic scoliosis, one group was treated during late onset of idiopathic scoliosis with the TLSO Boston brace and the second group was untreated. The groups were based on curve size, location, and age at diagnosis, furthermore, all were Risser sign 0 at diagnosis. Goldberg et al., (1993) found that there was no statistically significant difference between the groups on any parameter of curve progression (Cobb angle and vertebral column rotation). Therefore, doubts were raised about the efficacy of spinal orthoses in modifying the natural history of late-onset idiopathic scoliosis and removes the ethical problems inherent in a prospective trail in which the only treatment permitted to the control group is surgery.There are numerous studies on the effectiveness of braces in preventing the progression of the deformity, by taking the Cobb angle as the evaluated parameter, and occasionally the axial rotation angle as well (Mellencamp et al., 1977; Hopf and Heine, 1985; Liljenqvist et al., 1998) but the majority are not conclusive for several reasons. These reasons are related to the design of the retrospective studies, the heterogeneity of the specimens, including males, females, juvenile and adolescent scoliosis, with initial Cobb angles and also with a very variable initial bone age. The conclusive study on the effectiveness of the brace in preventing the progression of the Cobb angle is the study directed by Nachemson and Peterson, (1995). This is a prospective, controlled study, in which, patients were observed and placed in the control group, or treated by electro-stimulation or with a TLSO Boston-type brace. Although, TLSO Boston brace appears effective in preventing lateral curve progression, it does not necessarily mean 3D correction.
II) MILWAUKEE BRACE COMPARED WITH THE TLSO BOSTON BRACE
Long-term studies of both the Milwaukee and TLSO Boston brace have demonstrated that the main effect of orthotic treatment is to produce a curve that is only a few degrees better than that of the original deformity (Edmondson and Morris, 1977; Mellencamp et al., 1977). Therefore, it is assumed that bracing prevents deterioration but does not convert major deformities into normal physiological shapes.
III) TLSO BRACES COMPARED WITH NATURAL HISTORY
Miller et al., (1984) studied 255 female patients with initial curvature measuring 15-30 degrees and who ranged in age from 8 to 17 years. These patients were divided into two closely matched groups with 144 patients treated with various types of TLSO bracing and 111 patients going without active treatment. The results after a mean period of 1.9 years, suggested that bracing reduced the overall probability of progression when compared with the untreated group.
IV) TLSO COUPLING EFFECT
Aubin et al., (1996, 1997) reported that orthoses are widely used to treat scoliotic deformities of the trunk, but the way the corrective forces are transmitted from the thorax to the spine remains poorly understood, and several undesired effects such as the reduction of sagittal curvatures or weak derotations are often reported. A biomechanically measurable element model of the trunk was used to investigate the hypothesis that a coupling mechanism exists between the scoliotic spine and rib cage, which may explain incomplete and unexpected results obtained by orthotic treatments. Forces were applied to the model on the rib hump and lateral side of thorax. These biomechanical simulations demonstrated the existence of coupled motions between the spine and rib cage subjected to orthotic loads. Aubin et al., (1996, 1997) showed that reduction of physiological sagittal curvatures (up to 30%) are possibly related to anterior orthotic loads applied on the rib hump. These loads also contributed to increase lateral shift of the spine (up to 7 mm) as well as scoliotic frontal curvatures (up to 4 degrees). Based on these results, another approach was proposed and this consisted of applying loads laterally on the convex side as well as on the anterior thorax opposite to the rib hump, with a system that mechanically constrains the backward movement of the posterior rib hump. This biomechanical model was simulated on four scoliotic patients presenting thoracic curves between 22 and 54 degrees to evaluate its practicability. It was found that derotation of the trunk (7 to 13 degrees) and reduction of frontal curvatures could be done without reducing physiological sagittal curvature. More simulations on different scoliotic configurations are necessary to find the most optimal combination of forces to produce a real 3D correction of scoliotic deformities.Willers et al., (1993) demonstrated an undesirable effect of a reduction in the sagittal diameter of the thorax caused by the TLSO Boston brace. Labelle et al., (1996) and Aubin et al., (1996, 1997) reported that the TLSO Boston brace produces a lordotic effect (hypokyphosis) in the thoracic region as a result of the coupling of the spine and the ribs of the costal gibbus. This is caused by the forces acting from dorsal to the ventral aspect. The authors Labelle et al., (1996) and Aubin et al., (1996, 1997) have recently proposed a modification of the correction principles, which consists of applying loads laterally on the convex side as well as on the anterior thorax opposite to the rib hump, with a system that mechanically constrains the backward movement of the posterior rib hump. Indeed, these proposed modifications are not very different from those originally proposed by Chêneau, (1990, 1994, 1996a). The correction principles originally proposed by Chêneau in 1979 facilitate correction as a result of the location and size of the forces, as well as the expansion rooms on the opposite side of the convexities, which permit derotation, coronal plane correction and sagittal normalization.
V) CHÊNEAU BRACE STUDIES
A study by Oberthaler et al., (1985) was conducted on 115 patients with idiopathic scoliosis treated with either the TLSO Boston brace or the Chêneau brace. The results found that there was excellent Cobb angle correction of the deformity in both braces. The TLSO Boston brace seems to be better for lumbar and thoracic curves whereas the Chêneau brace lends itself more for thoracic curves or when more than one primary curve is present. It was also claimed that the TLSO Boston brace was effective in treatment of mild hyperkyphosis.Von Deimling et al., (1995) compared long-term influence of idiopathic scoliosis in 47 patients who wore either the Milwaukee brace or the Chêneau brace with an average follow-up of 7.8 years. It was reported that Chêneau brace had significantly better results. There was a Cobb angle correction of 62% and 38% the patients who wore the Chêneau and Milwaukee braces respectively. The initial correction of the Cobb angle was 35% and 47% of the pre-treatment value in the Chêneau and Milwaukee braces.Rigo (1999c) reported a retrospective study of 105 patients (mean age of 12.5 years) with progressive idiopathic scoliosis who were treated with the Chêneau brace. Of this group, 44 patients had been wearing other braces from other clinics before the start of treatment with the Chêneau brace. All of these 44 patients presented curve progression even while wearing their previous brace. The major Cobb and torsion angles had a mean of 37 degrees and 17 degrees respectively at the start of Chêneau brace treatment. The major Cobb and torsion angles had a mean primary correction of 31% and 22% respectively. In the group of patients with end results (n=37) the mean initial major Cobb and torsion angles were 36.4 and 16.9 degrees respectively and at follow-up they were 34.1 and 15.7 degrees. The results show high initial Cobb angles at the start of treatment and a low primary correction. The final Cobb angle at a 2-year follow-up, showed a tendency of a loss of correction, without reaching significance. Rigo (1999c) claimed that the Chêneau brace could effectively prevent the progression of the Cobb and torsion angles, even in cases of bad prognosis. In agreement with other authors, these results show better end results with a low initial Cobb angle and high primary correction. The primary correction is less than those of Hopf and Heine, (1985) as well as Liljenqvist et al., (1998) however this could be due to the higher initial Cobb angle and poor effect of previous treatments of lower quality braces producing more rigid curves.
VI) CHÊNEAU BRACE
Dr. Chêneau, inspired by Abbot, fabricated the original Chêneau brace in 1979. The Chêneau brace is commonly used for the treatment of scoliosis and thoracic hypokyphosis in many European countries such as Spain, France, and Germany as well as other countries like Israel and Russia. However, it is not commonly prescribed in North America and the UK.
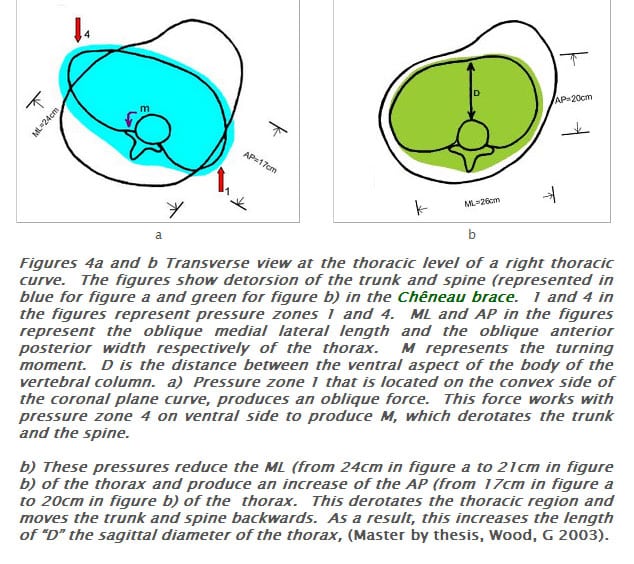
The brace is fabricated in polypropylene and has an anterior opening with Velcro straps for fastening. The Chêneau brace is defined as a thermoplastic brace modelled on a hyper-corrected positive plaster mould of the patient. The general correction principle is that of detorsion and sagittal plane normalisation, which would correct the coronal and transversal planes, resulting in some elongation of the spine, without any significant distraction force, (Rigo, 1999a).
The objectives of the Chêneau brace are to obtain a three-dimensional correction of the scoliotic deformity, with emphasis not only on the coronal and transverse planes, but also on the sagittal plane (Matthiass and Heine, 1984; Syndikus et al., 1988; Giorgi et al., 1996; Losito et al., 1996; Kotwicki et al., 1999).
The deformation of the scoliotic body consist of (Chêneau 1996a, 1996b):
- The paired convexities and concavities: in an oblique plane the brace reduces the convexities and transfers tissues from the convex humps in the direction of the concave flat areas. All abnormal protrusions with respect to the normal physiological shape must be submitted to pressure.
- Sagittal configuration deformity: often, abnormal thoracic kyphosis and lumbar lordosis is presented in the scoliotic patient.
- Torsion of the pelvis and rotation of the shoulders: the brace must produce a detorsion of the pelvis and derotation of the shoulders.
- The lateral displacement: in a transverse plane the brace establishes a balance of the shoulders and thorax over the sacrum.
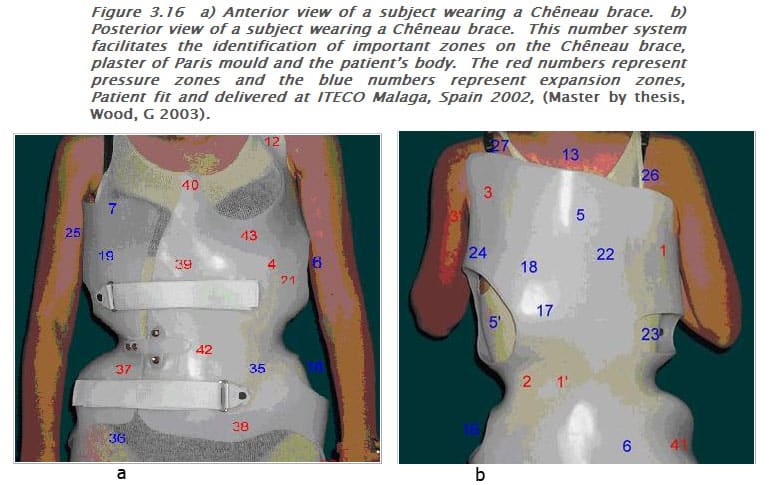
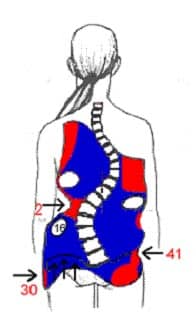
Chêneau (1990) provided a number system to indicate pressure and expansion zones on the Chêneau brace. This number system facilitates the identification of important zones on the Chêneau brace, plaster of Paris cast and the patient’s body (figure 3.16a and b). The system lists number 1 through number 43, however some numbers are missing as the evolution of the brace has made them obsolete. The number system is used in all different types of classifications of scoliosis and curves, hence it is not limited to only one type of curve. However, not all the numbers in this number system are utilised in all cases. This is because sometimes a particular number may not be utilised as its corresponding function is not required.
Additionally, the location of the numbers often change from being on the right side of the brace to the left side and vice versa, as each scoliosis case is treated independently. As a result, the locations of these numbers are often determined by the direction of the curve convexity. Therefore the brace design is different for each individual case. The basic location of the pressure and expansion zones using the Chêneau brace number system and their corresponding functions are indicated below.
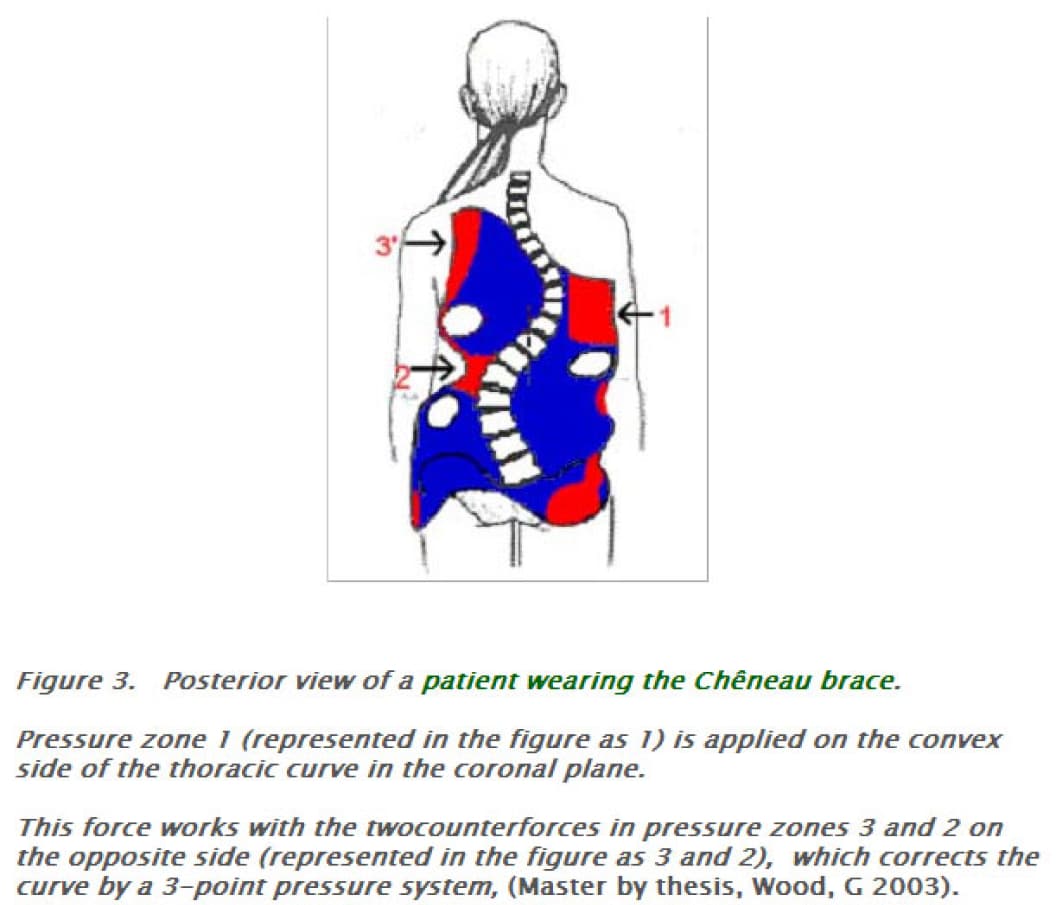
1: The location of the pressure zone 1 is on the convex side of the thoracic or thoracolumbar curve on the dorsal aspect of the brace. The function of this pressure is for the correction of the thoracic or thoracolumbar curve in the coronal plane and rotation of the vertebral column in the transverse plane.
1´: The location of pressure zone 1´ is on the convex side of the lumbar curve on the dorsal aspect of the brace. This pressure zone is extended to the posterior midline in the case of lumbar hypolordosis, which is for the correction of the deformity in the sagittal plane.
2: The location of the pressure zone 2 is on the convex side of the lumbar curve on the dorsal aspect of the brace. The function of this pressure is for the correction the lumbar curve in the coronal plane and if present, correction of the lumbar hypolordosis deformity in the sagittal plane.
3´: The pressure zone 3´applies a counterforce to the axilla that works on the opposite side to zone 1, which is for the correction of the thoracic and thoracolumbar curve in the coronal plane. Also, in the case of an unbalanced trunk over the pelvis, this force pushes the trunk to the midline of the body, placing it over the pelvis. When retropulsion of the shoulder is present, this force lifts the lower shoulder superiorly.
3: The location of pressure zone 3 is at the same level as 3´, but it is more posteriorly placed to move the retropulsion shoulder ventrally in the sagittal plane.
4: The location of pressure zone 4 is on the ventral aspect of the trunk. This force is placed adjacent to the pressure zone 1. The function of these forces is to work together to reduce the large diameter of the oval shaped thorax, which facilitates the derotation of the thoracic region in the transverse plane.
5: The location of expansion zone 5 is beside the thoracic and thoracolumbar curve and pressure zone 1. The function of this expansion zone is to provide a room or space for the expansion of the trunk, which allows respiratory movement, and permits small voluntary and involuntary movements as well as the patient’s growth. This provides an active mechanism of correction in the direction of derotation and rekyphosis,
5´: The location of this expansion zone is on the concave side of the thoracic curve and is opposite to pressure zone 1. The function of this expansion zone is to provide a room or space for the expansion of the trunk, which corrects the thoracic curve in the coronal plane.
6: The location of expansion zone 6 is on the posterior aspect of the hemipelvis that is in anteversion. This provides a space for the derotation the hemipelvis.
7: The location of expansion zone 7 is on the ventral aspect and is adjacent to pressure zone 3. The function is to provide a large space for the correction of the rotation and hypokyphosis of the thoracic region.
12: The location of pressure zone 12 is in the subclavicular region of the lower shoulder, which is positioned in retropulsion. The function is to facilitate control of the retropulsion shoulder in the sagittal plane.
13: The location of expansion zone 13 is outside the dorsal superior trimline of the brace above expansion zone 5. Its function is to provide an expansion zone for the correction of the thorax.
17: The location of expansion zone 17 is on the dorsal aspect of the brace next to expansion zone and window 5´ . Its function is to provide an expansion zone for the correction of the thoracic or thoracolumbar curve.
18: The location of expansion zone 18 is on the dorsal aspect of the brace above expansion zone and window 5´ . Its function is to provide an expansion zone for the correction of the thoracic or thoracolumbar curve.
19: The location of expansion zone 19 is on the breast that is tilted to the high side. The function is to provide a large space for the correction of rotation and hypokyphosis of the thoracic region.
21: The location of pressure zone 21 is on the ventral aspect between pressure zone 4 and pressure zone 2. The function is to connect pressure zone 4 and pressure zone 2. This provides a smooth connection of the pressure zones and forces from the body to the brace, also this gives a more cosmetic appearance.
23: The location of this expansion zone 23 is on the concave side of the lumbar curve and is opposite to pressure zone 2. The function of this expansion zone is to provide a room or space for the expansion of the trunk, which corrects the lumbar curve in the coronal plane.
24: The location of expansion zone 24 is on the dorsal aspect of the brace above expansion zone and window 5´ and ventral to expansion zone 18. Its function is to provide an expansion zone for the correction of the thoracic or thoracolumbar curve
26: The location of expansion zone 26 is outside the dorsal superior trimline of the brace above pressure zone 1. Its function is to provide an expansion zone for the correction of the thorax.
27: The location of expansion zone 27 is on the concave side of the thoracic or thoracolumbar curve, just above pressure zone 3 on the shoulder, which is in the position of retropulsion. The function of this zone is to provide an expansion zone for the shoulder in retropulsion.
30: The location of pressure zone 30 is applied to the greater trochanter on the low side of the pelvic tilt. The function of this force is to work with pressure zone 2, which provide counterforces to pressure zone 41 to move the pelvis upward from its tilted position.
33: The location of expansion zone 33 is on the dorsal inferior aspect of the brace, which is in retroversion. The function is to allow space for the derotation of the hemipelvis, which is in retroversion in the sagittal plane.
34: The location of the pressure zone 34 is on the dorsal inferior aspect of the brace, which is in anteversion, at the level of the gluteus maximus. The function of this force is to derotate the hemipelvis, which is in retroversion in the sagittal plane.
35: The location of expansion zone 35 is on the low side of the pelvic tilt, positioned on the ventral inferior aspect of the brace. This is above pressure zone 30 at the level of the iliac crest. The function is to provide room or space for the derotation of the hemipelvis in retroversion by allowing it to move upward.
36: The location of expansion zone 36 is on the ventral side of the body, in which the hemipelvis is in anteversion, below pressure zone 37. The function is to allow space for the derotation of the hemipelvis, which is in anteversion in the sagittal plane.
37: The location of the pressure zone 37 is along the waistline going downward towards the ASIS (anterior superior iliac spine) on the side of the body that has the hemipelvis in anteversion. The function of this pressure zone is to derotate the anteversion position of the hemipelvis in the sagittal plane.
38: The location of the pressure zone 38 is above the symphysis pubis on the same side of the body that has the hemipelvis in retroversion. The function of this force is to derotate the retroversion position of the pelvis.
39: The location of the pressure zone 39 is on the ventral aspect of the brace and is below pressure zone
40. The function of this force is to reduce the distance of the oval thorax, this corrects the hypokyphosis in the sagittal plane by causing flexion of the thoracic vertebral column.
40: The location of the pressure zone 40 is on the ventral aspect of the brace and is adjacent to the pressure zone 1, which is on the convex side of the thoracic or thoracolumbar curve. The function of this force is to reduce the distance of the oval thorax, this corrects the hypokyphosis in the sagittal plane by causing flexion of the thoracic vertebral column.
41: The location of the pressure zone 41 is in the iliac fossa, on the lateral aspect of the hemipelvis, which is on the high side of the pelvic tilt. The function of this force is to work with pressure zone 30 and pressure zone 2 to provide a 3-point pressure system that lifts the low contralateral hemipelvis.
43: The location of the pressure zone 43 is underneath the lower positioned breast, which lifts it to the level of the contralateral breast. In the case of a male patient, this zone is designed the same way as the female patient, however it would not have to be as large. The function of this zone is to balance the lower positioned breast with the contralateral side.
Thoracic Section
The objectives of the thoracic section are to correct the coronal plane curve, derotate the thoracic vertebral column and obtain a more normal physiological sagittal configuration, (Chêneau, 1996a, 1996b; Chêneau et al., 1997). The trimlines in the thoracic section, which are located on the posterior superior aspect of the brace, have an asymmetrical shape. Pressure zone 1 is applied two vertebras above and two vertebras below the apex on the convex side of the thoracic or thoracolumbar curve, (figure 2). Its shape in the transversal plane is oblique and is applied in the dorsal lateral aspect of the patient’s back. The function of this pressure is for the correction of the thoracic or thoracolumbar curve in the coronal plane and rotation of the vertebral column in the transverse plane (figure 3).
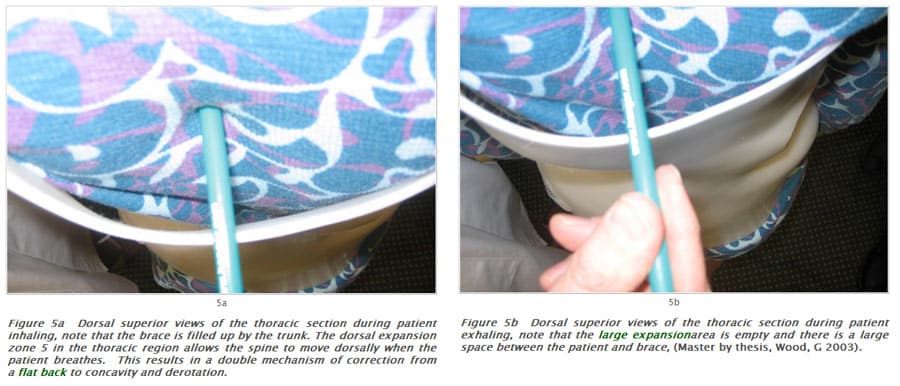
Pressure zones 1 and 4 reduce the larger diameter of the thorax and increase the smaller diameter. These actions reduce the humps and fill-in the flat areas. This dorsal displacement of the spine, fills in the dorsal expansion zone 5 (figure 5a), as a result, this reduces the thoracic hypokyphosis. The dorsal thorax is not in contact with the brace, however, the space is important for respiratory movement, and permits small voluntary and involuntary movements as well as the patient’s growth. This provides an active mechanism of correction in the direction of derotation and rekyphosis.
Lumbar Section
The lumbar section consists of pressure zones 2 and 1´ , which are applied one vertebra above and one vertebra below the apex of the lumbar curve. These dorsally located pressures are a continuation from the ventral pressure zone 4. Pressure zone 1´ extends almost to the posterior midline when lumbar hypolordosis is present and thus, it is needed to influence normal lumbar lordosis. In the case that it is not required to increase the lordosis, pressure zone 1´ is not utilised, and the pressure zone 2 extends less to the midline. The shape of these pressures are smooth and sufficiently deep enough to apply a corrective force to the lumbar curve.
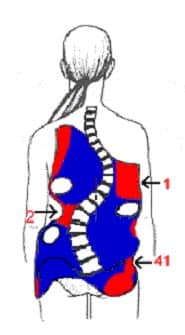
The function of pressure zone 2 is for the lumbar curve correction in the coronal plane. The 3-point pressure system is made up of pressure zone 2 and the counterforces from pressure zones 1 and 41. Pressure zone 2 is applied above and below the apex of the curve, pressure zone 1 is a counterforce which is applied to the opposite side of the lumbar curve and is located cephalically to the apex. Pressure zone 41 is also applied to the opposite side of the lumbar curve and is located caudally to the apex, which is below the iliac crest, as shown in figure 3.21.
Pelvic Section
The pelvic section is designed to correct pelvic tilt and pelvic torsion. The pelvic tilt presents as a protrusion of the pelvis. Usually, the hemipelvis is higher on the thoracic convex side. The pelvic tilt is corrected by a 3-point pressure system that consists of pressure zones 41, 2 and 30 and expansion zone 16. The location of pressure zone 41 is on the iliac fossa, which is on the high side of the pelvic tilt. Pressure zone 2 is on the opposite side to pressure zone 41 and is located approximately 3cm above the iliac crest. Pressure zone 30 is on the opposite side to pressure zone 41, and is located on the greater trochanter. Expansion zone 16 has a window and is required on the low side of the hemipelvis. This provides a space for the hemipelvis to move into during correction.
Pressure zone 41 has a concave shape, which mimics the anatomical dimple-shape of the iliac fossa. Its inferior lateral trimline is at the caudal aspect of the iliac fossa. The pressure zone 30 is shaped so as to apply slight pressure on the greater trochanter, without causing discomfort. The trimline extends to the greater trochanter so that the counterforce works with pressure zone 2. Pressure zone 2 is shaped as previously mentioned in the lumbar section. The pelvic grip of the brace is designed so that it is higher on the side in which the pelvis is tilted lower, hence it has an asymmetrical shape.
The functions of these forces are to work together as a 3-point pressure system. Pressure zone 41 pushes the contralateral hemipelvis upward and the expansion zone 16 provides a space for the hemipelvis to move into for correction, (figure 3.22).
Pelvic torsion consists of iliac rotation and pelvis transversal rotation. The iliac rotation refers to a position of relative anteversion of the concave side of the lumbar curve and retroversion of the convex side of the lumbar curve. Anteversion is an abnormal position of the hemipelvis that is rotated and torsioned anteriorly therefore the ASIS is more prominent than usual, (figure 3.23). The contralateral hemipelvis would be in retroversion. Retroversion is an abnormal position of the hemipelvis, which is rotated and torsioned posteriorly therefore the ASIS is less prominent than usual, (figure 3.24). The contralateral hemipelvis would be in anteversion.
Rigo and Chêneau (1997, 2000) reported that this could be the consequence of passive tension of the lumbar fascicles of the erector spinae (longisimus thoracis and iliocostalis). Rigo (1999a) found that sometimes, combined or substituting iliac rotation causes a true three-dimensional iliac torsion (a bone deformity). Iliac rotation is corrected by pressure zones 37 and 34 as well as expansion zones 36 and 6 on the hemipelvis that is in anteversion. Pressure zones 38 and 2 as well as expansion zones 35 and 33 are applied to the hemipelvis that is in retroversion. Also by correction of the lumbar curve, the pelvis automatically assumes an anteversion position and therefore corrects itself.
The hemipelvis that is in anteversion, has its ventral inferior trimline of the brace that extends inferiorly to cover the ASIS and pressure zone 37. However it is not as low as the contralateral side because expansion is required by expansion zone 36 for the correction of anteversion. The dorsal inferior trimline, for the same hemipelvis, extends inferiorly to the gluteus maximus. This trimline is sufficiently inferior to apply pressure zone 34.
The hemipelvis that is in retroversion, has its ventral inferior trimline of the brace that extends inferiorly to above the symphysis pubis to apply pressure zone 38. This is much lower than the contralateral side because pressure is required by pressure zone 38 for the correction of retroversion. The dorsal inferior trimline, for the same hemipelvis, is higher than the contralateral side because expansion is required by expansion zone 33 for the correction of retroversion. These inferior ventral and dorsal trimlines are asymmetrical and depend on the position of the pelvis.
|
Figure 3.22 Posterior view of a right thoracic and left lumbar curves in the coronal plane. Pressure zones 41, 2, 30 and expansion zone 16 are represented in the figure as 41, 2, 30 and 16 respectively. The upward moment is represented as M. The thoracic convexity is to the right, therefore the pelvis tilt is to the left side. Pressure zone 41 pushes the pelvis between the two counterforces 2 and 30, therefore M is produced. This moves the left hemipelvis upward into expansion zone 16, as a result the pelvis is levelled, (Master by thesis, Wood, G 2003). |
Chapter I
AIMS AND OBJECTIVES
The aims of this thesis are to conduct a comparative study of surface topography and X-ray angles in idiopathic scoliosis before and after treatment with the Chêneau brace.
Therefore, the primary objectives of this project were to:
- To evaluate the following topography values using the Formetric system: lateral deviation, rotation and trunk length before and after Chêneau brace treatment.
- To identify the subject’s Cobb and rotation angles using the X-ray measurements and evaluate the correction of scoliosis by comparing measurements before and after treatment with the Chêneau brace.
- To evaluate a cross-correlation of subjects who present Cobb angles less than 30 degrees and 30 degrees or greater compared with those subjects who present a Risser sign 0 or 1 and those subjects who present a Risser sign 3.
- To evaluate the topographical parameters of those subjects who had no previous brace treatment, with previous brace treatment, using Chêneau classification and King type patterns.
Chapter II
INTRODUCTION
The medical team’s desire to provide a more active and three-dimensional (3D) scoliosis brace, as well as the introduction of thermoplastics, have allowed for a proliferation of advances in scoliosis braces. Currently the thoracolumbosacral orthosis (TLSO) Boston brace is considered the “gold standard”, and has superseded the conventional Milwaukee brace, which has been for many years the industry standard.
Thermoplastic braces such as the TLSO Boston brace places pressure pads over the convexities of the thoracic and lumbar curves in attempt to correct lateral deviation and rotation. However, Dr. Chêneau in 1979 found these general correction principles insufficient, and as a result, he designed a Chêneau brace that endeavours to treat every aspect of the complex 3D deformity (Rigo and Chêneau, 1997). The Chêneau brace is defined as a thermoplastic brace modelled on a hyper-corrected positive plaster-cast of the patient. The general correction principle is that of detorsion and sagittal plane normalisation, which would correct the coronal and transverse planes, resulting in some elongation of the spine, without any significant distraction force. However, due to the complexity of rectification and fitting processes, it has been limited to specialised clinics in Europe.
2.1 ANATOMY OF THE VERTEBRAL COLUMN
The spine can be divided into anterior and posterior columns. The anterior column consists of the posterior longitudinal ligament, intervertebral disc, vertebral body, and anterior longitudinal ligament. The elements of the posterior column are the pedicles, laminae, transverse processes, spinous process, facet joints, and ligamentous structures, including the facet joint capsule, ligamentum flavum, intertransverse ligaments, interspinous ligaments, and supraspinous ligaments. Each anatomic component of the vertebral column has a function that contributes to the mobility and stability of a motion segment (Verbout, 1985; Lonstein et al., 1995).
2.2 PHYSIOLOGY OF THE VERTEBRAL COLUMN
The normal adult vertebral column has four curvatures in the sagittal plane, a convexity (lordosis) in the cervical and lumbar regions and a concavity (kyphosis) in the thoracic and sacrococcygeal regions. In the coronal plane, the vertebral column is normally straight. In the sagittal plane, both the cervical and lumbar curvatures are acquired in late foetal development when the infant begins to hold up its head to enlarge its visual environment. The secondary lumbar curvature appears when the child begins to sit up at around 6 months, becoming more marked with standing and the onset of walking. It is the extension of the hip, which accompanies standing and walking which tilts the pelvis forwards so that the axis of the pelvic cavity is no longer in line with that of the abdominal cavity. The lumbar curvature develops in order to keep the trunk erect when standing. The lumbar curvature is not fully developed until after the age of two, when a more or less adult pattern of walking is established. In old age, the vertebral column tends to assume a gentle C-shaped curve, which is reminiscent of the fetal curve. The reason for this is that the shape of the vertebral column is largely determined by the intervertebral discs and to a much lesser extent by the vertebras themselves. Consequently as the discs degenerate and become thinner with increasing age, the secondary curvatures gradually disappear (Netter, 1985; Palastanga et al., 1990).
2.3 BIOMECHANICS OF THE VERTEBRAL COLUMN
Humans have an axial skeleton uniquely adapted to bipedal ambulation (White and Panjabi, 1978). Sagittal plane contours permit the centre of mass for the head and upper torso to remain in line with the vertical axis through the centre of mass for the pelvis; therefore, a minimal expenditure of energy is required to keep the trunk upright. The upper limbs, thus freed from the task of trunk support, are able to perform other functions associated with a complex society. Various pathologic conditions causing abnormal sagittal plane contour, such as loss of lumbar lordosis, excessive thoracic kyphosis, or coronal plane deviation of the spine, may alter balance and coordination, interfere with visceral function, allow premature degeneration of the intervertebral disc and facet joints, and cause deterioration of neurologic function, (Netter, 1985; White and Panjabi, 1990).
To achieve the balance and mobility required for efficient energy use, humans have a multisegmented, bony spinal column. The normal spinal column consists of 7 cervical, 12 thoracic, and 5 lumbar vertebrae connected to fused sacral vertebrae, in turn, articulate with vestigial coccygeal vertebrae. When viewed in the coronal plane, the normal spinal contour has less than 10 degrees of lateral curvature and when viewed in the lateral plane it has physiologic cervical lordosis, thoracic kyphosis, and lumbar lordosis (White and Panjabi, 1978, 1990).
In mechanical terms, the vertebral column can be modelled as a series of semi-rigid bodies, the vertebras, separated by viscoelastic linkages and the intervertebral discs and ligaments (Pearcy, 1989). Attached to the vertebral column are various viscoelastic and solid materials with varying mechanical properties. They vary from the stiff ribs associated with the thoracic region, to the subcutaneous fat. These elements form part of a body cylinder, to which the spinal brace or orthosis is applied. The effectiveness of a spinal brace can be assessed in biomechanical terms, whether the main function is one of support, immobilisation, correction and/or pain relief. The nature of the close-fitting orthosis establishes externally applied forces that are transmitted to the vertebral column to obtain the desired therapeutic goal. The effectiveness of the force transmission from the orthosis to the vertebral column is determined by the mechanical properties of the human body, in particular the stiffness characteristics of the intervening biological materials. Therefore it is more effective when the applied forces are directed through a rigid material that deforms minimally under pressure compared with less rigid material that can deform under pressure. It can be seen why a spinal brace is more effective in holding or correcting thoracic curves, where the forces are transmitted through the ribs, compared with the lumbar curves where the intervening soft materials are composed of muscles and viscera (White and Punjabi, 1990; Chase et al., 1993).
2.4 LITERATURE REVIEW
2.4.1 AETIOLOGY OF IDIOPATHIC SCOLIOSIS
By definition, the cause of idiopathic scoliosis is unknown (Lonstein et al., 1995). Although research has possibly eliminated some hypothetical causes, abnormalities of disc, bone, muscle, and collagen do not appear to be aetiological factors (Abbott-Byrd, 1988; Child et al., 1999; Miller et al., 1999). However they reflect the effects of scoliosis on normal tissues (Abbott-Byrd, 1988). Idiopathic scoliosis is the most common type of lateral deviation of the spine (Abbott 1912), and as a result, this has prompted many lines of research, which focus on the genetic aspects (Fillio and Thompson 1971; Miller et al., 1999), growth aspects (Skogland and Miller 1980; Duval-Beaupere, 1970, 1992), structural and biochemical changes in the discs and muscle (Riddle and Roaf, 1975; Taylor et al., 1981; Drummond et al., 1984; Child et al., 1999), and on central nervous system changes (Willner, 1972; Yamada et al., 1974).
Family and population studies point to a hereditary factor to explain the well-known familial pattern (Cowell et al., 1969), however the mode of inheritance is uncertain.
I) CURVE PROGRESSION
Growth has a definite role in idiopathic scoliosis. Curves progress rapidly during the adolescent growth spurt, which occurs at the age of 12 years in girls and at 13 or 14 in boys (Duval-Beaupere, 1970; Stokes, 1999). Willner (1975) reported that idiopathic scoliosis is intimately associated with growth and development, particularly during the beginning of puberty, when the rate of growth is at a maximum. Moe (1969) claimed that the crucial year in girls is the year before menarche, (the onset of menstruation). It is at this time that the risk of progression of the spinal curvature is at its greatest. The Swedish study of Nordwall and Willner (1975) showed that teenage girls with idiopathic scoliosis had a skeletal age, which in early adolescence was more advanced than normal, and a menarche which did not differ from that of normal girls.
II) EFFECT ON GROWTH
Drummond et al., (1984) reported in 409 adolescents with idiopathic scoliosis that growth of children with scoliosis did not appear to differ from that of their peers. However, when growth was compared with skeletal age, the children with scoliosis were found to be taller and heavier. Both boys and girls with scoliosis showed a significant tendency for a delay in skeletal age and the girls showed a significant tendency for a delay of puberty. The late skeletal and sexual development observed for the entire series was even more apparent for the girls with a Cobb angle greater than 20 degrees.
In another Swedish study, Willner (1975) found that girls with adolescent idiopathic scoliosis were significantly taller than their normal peers. These girls started their growth spurts earlier, grew for a longer period and had a skeletal age more advanced than their normal peers. At the end of growth, the heights of the girls with scoliosis and their normal peers were equal. The levels of growth hormone in girls with scoliosis were compared to normal, and some studies showed an increase in these levels, however Misol et al., (1971) could not confirm this finding.
Investigations into collagen in the ligaments and tendons in patients with idiopathic scoliosis were compared to normal, but no differences were found (Waters and Morris, 1973; Lonstein et al., 1982,). Muscles have been implicated as the cause of idiopathic scoliosis however electromyographic studies have been inconclusive (Zuk, 1962; Riddle and Roaf, 1975). Increased activity on the convexity has been found by some investigators (Butterworth and James, 1969; Sahlstrand and Petruson, 1979), whereas others found no difference (Henssge, 1967; Lihvar et al., 1975). Postural equilibrium dysfunction has been found by many authors (Herman et al., 1979; Willner, 1982), and these findings were not specific for idiopathic scoliosis. It appears that there may be a postural equilibrium problem in idiopathic scoliosis and some authors have suggested that this may be due to the brainstem.
The cause of idiopathic scoliosis is still unknown, however despite numerous studies that have been done on the subject, it appears that the cause is multifactorial, as no single causative factor can be found (Czeizel et al., 1978; Aksenovich et al., 1988). Genetic, growth, chemical, biomechanical and neuromuscular factors all seem to be involved (Willner, 1982; Child et al., 1999). It has also been postulated that a mild central nervous system abnormality is genetically determined. With increased growth and the altered viscoelasticity of the discs, the spine is biomechanically less stable, making it susceptible to changes in postural equilibrium. The interrelation of all these factors determines whether the curve is progressive or nonprogressive, and how much progression will occur (Lonstein et al., 1995).
III) PREVALENCE
Prevalence refers to the number of the population with the disease or disorder, therefore when discussing scoliosis, the studies give prevalence rates. Prevalence rates vary as to the degree of Cobb angle, being 20 to 30 cases per 1000 individuals for curves over 10 degrees Cobb angle. The number of cases reduces to three to five cases per 1000 for curves over 20 degrees Cobb angle and two to three per 1000 for curves over 30 degrees Cobb angle (Shands and Eisberg, 1955; Dickson et al., 1980;
Willner, 1982). Therefore, the prevalence of idiopathic scoliosis decreases when a larger curve magnitude is considered. A study in Edinburgh of 153 patients with idiopathic scoliosis showed that 4% had infantile, 7% had juvenile, and 89% had adolescent idiopathic scoliosis (McMaster, 1983). Mau (1981), in Germany as well as Riseborough and Wynne-Davies (1973), in North America found similar frequencies in idiopathic scoliosis.
2.4.2 NATURAL HISTORY OF ADOLESCENT IDIOPATHIC SCOLIOSIS
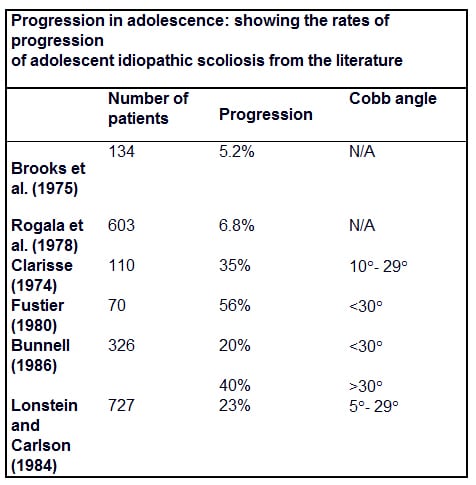
Much work has been done on the negative effects of untreated scoliosis, which involves back pain, cardiopulmonary problems and socio-economic effects (Nachemson, 1968, 1996; Weinstein et al., 1981). The progression rates (in which the Cobb angle increases five degrees or more during a six-month period), are fairly well documented for adolescent idiopathic scoliosis and these vary from 5.2% to 56% (Clarisse, 1974; Brooks et al., 1975; Rogala et al., 1978; Fustier, 1980; Lonstein and Carlson, 1984; Bunnell, 1986), with the lower rates being found in school screening studies (table 2.1).
The factors that are related to the risk of curve progression are divided into two groups, those of curve magnitude and growth potential. Firstly, the factors related to the curve magnitude, such as whether the curve is 25 to 29 degrees or over 30 degrees, are evaluated. Secondly, those related to the child’s growth potential, such as age, skeletal maturity, menarchal stage (Peterson and Nachemson, 1995), and the stage of development of the apophysis of the iliac crest (the Risser sign (Risser, 1958, 1964)). Generally the larger the Cobb angle, the greater the incidence of progression. This also varied with the curve pattern (Clarisse, 1974). Lonstein and Carlson (1984) found that, in curves between 5 and 29 degrees, the incidence of progression in the different curve patterns was fairly equal, except for the single lumbar and single thoracolumbar pattern. Therefore, a double curve is more likely to progress than a single curve (Lonstein et al., 1995; Peterson and Nachemson, 1995).
When analysing the growth potential and curve progression, it is generally true that the younger the child (i.e. the greater the growth potential), the greater the incidence of progression (Goldberg et al., 1993; Lonstein et al., 1995; Peterson and Nachemson, 1995). This can be measured by age (chronological or skeletal), menarchal status, or Risser sign. The Risser sign (Risser, 1958, 1964), is measured by the ossification of the iliac epiphysis (figure 2.1). Ossification normally starts at the anterior superior iliac spine (ASIS) and progresses posteriorly to the posterior superior iliac spine (PSIS). Risser divided the excursion into four quarters, Risser sign 1 through 4, with Risser sign 5 once complete ossification has occurred in which fusion to the iliac crest takes place. The incidence of progression is higher in adolescents with a Risser sign of 0 or 1, compared to those with a Risser sign of 2 or more (Lonstein et al., 1995).
Figure 2.1 Coronal plane view of the pelvis and the 4th and 5th lumbar vertebrae which presents iliac epiphysis. Ossification of the epiphysis usually starts at the anterior superior iliac spine and progresses posteriorly. The iliac crest is divided into four quarters, and the excursion or stage of maturity is designated as the amount of progression. In the example shown, the excursion is 50 per cent complete, and the Risser sign is thus 2+. On the right, the excursion is complete and the epiphysis has fused with the iliac crest, this is a Risser 5+.
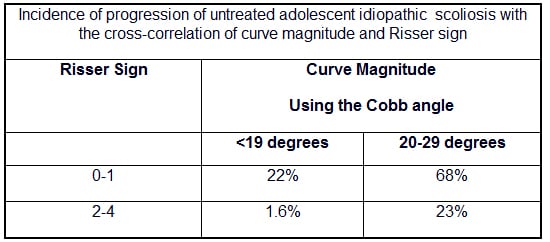
A useful cross-correlation of incidence rates of progression for curves under 29 degrees was reported by Lonstein et al., (1995). The two factors taken were the curve magnitude and maturity as assessed by the Risser sign (table 2.2). These figures are used for the natural history of incidence of progression when evaluating the effectiveness of treatment.
When analysing the growth potential and curve progression, it is generally true that the younger the child (i.e. the greater the growth potential), the greater the incidence of progression (Goldberg et al., 1993; Lonstein et al., 1995; Peterson and Nachemson, 1995). This can be measured by age (chronological or skeletal), menarchal status, or Risser sign. The Risser sign (Risser, 1958, 1964), is measured by the ossification of the iliac epiphysis (figure 2.1). Ossification normally starts at the anterior superior iliac spine (ASIS) and progresses posteriorly to the posterior superior iliac spine (PSIS). Risser divided the excursion into four quarters, Risser sign 1 through 4, with Risser sign 5 once complete ossification has occurred in which fusion to the iliac crest takes place. The incidence of progression is higher in adolescents with a Risser sign of 0 or 1, compared to those with a Risser sign of 2 or more (Lonstein et al., 1995).
Figure 2.1 Coronal plane view of the pelvis and the 4th and 5th lumbar vertebrae which presents iliac epiphysis. Ossification of the epiphysis usually starts at the anterior superior iliac spine and progresses posteriorly. The iliac crest is divided into four quarters, and the excursion or stage of maturity is designated as the amount of progression. In the example shown, the excursion is 50 per cent complete, and the Risser sign is thus 2+. On the right, the excursion is complete and the epiphysis has fused with the iliac crest, this is a Risser 5+.
A useful cross-correlation of incidence rates of progression for curves under 29 degrees was reported by Lonstein et al., (1995). The two factors taken were the curve magnitude and maturity as assessed by the Risser sign (table 2.2). These figures are used for the natural history of incidence of progression when evaluating the effectiveness of treatment.
Table 2.2 The prediction of curve progression in untreated idiopathic scoliosis during growth (Lonstein et al., 1995).
For curves of 20 to 29 degrees in an immature child with a Risser sign of 0 or 1, the incidence of progression was 68 %. On the other extreme, for curves less than 19 degrees in a mature adolescent with a Risser sign of 2 or more the incidence of progression was 1.6%. In the other two groups, that is, a smaller curve (less than 19 degrees) in an immature child (Risser 0 or 1), and a larger curve (20 to 29 degrees) in a mature child (Risser 2 or more), the incidence of progression is approximately the same at 22% to 23% (Lonstein et al., 1995).
Bunnell (1988), reported that a large number of patients have minor degrees of curvature (approximately 100 per 1000 patients), although only about two per 1000 patients warrant treatment because of curve progression. As a result, a large number of these curves do not increase even without treatment.
Kehl and Morrissy (1988) reported that, in the past, the majority of idiopathic curves in patients who presented for treatment were of a greater magnitude (40 to 60 degrees) than what is seen today. This is because school screening programs becomes more prevalent and a large number of patients with smaller curves (10 to 30 degrees) have been identified. Past experience also indicated that idiopathic scoliosis was a disease of relentless curve progression. Kehl and Morrissy, (1988), assumed that without early treatment, curves that had progressed to 20 degrees would continue to progress and subsequently become the larger curves that normally constituted the bulk of scoliosis practice. As bracing was aimed at preventing the progression of scoliosis as all curves were assumed to be progressive, it was logical to begin brace treatment early for all small curves. This concept of treating all 20-degree curves with a brace was supported by initial reports that showed a high rate of success in controlling progression (Kehl and Morrissy, 1988). This was an erroneous assumption demonstrating the fallacy of evaluating the treatment of a disease in which the natural history was not known. Statistics from school screening studies would soon change this concept (Edgar et al., 1982; Goldberg et al., 1993; Peterson and Nachemson, 1995; Lonstein et al., 1995).
Kehl and Morrissy (1988) claimed that although the understanding of the natural history of adolescent idiopathic scoliosis has increased, it remains incomplete. This information implies that the high rate of success seen in bracing in idiopathic curvature was more likely to be secondary to the favourable natural history associated with these cases than the effects of wearing a brace. It also implies that the frequency of the need for bracing is much less than has previously been proposed (Kehl and Morrissy, 1988).
Therefore, by claiming that if all idiopathic curves less than 25 degrees were routinely braced, simply to prevent a progression from occurring, then a very large percentage of patients treated would be braced unnecessarily. This unnecessary bracing would subject many adolescent patients and their families to unneeded financial cost and potential psychological harm without adding any potential benefit to the patient’s final outcome (Kehl and Morrissy, 1988).
Goldberg et al., (1993) found that observation of progression of at least 10 degrees, which occurred in 14% of the group of 339 girls with adolescent idiopathic scoliosis, depended on the timing of diagnosis and related primarily to the child’s position on her growth rate curve as well as her pubertal status, and much less to her skeletal maturity as interpreted by iliac crest ossification or bone age.
2.4.3 PHYSIOTHERAPY
Physiotherapy programs such as the Schroth technique have been advocated as a necessary part of brace treatment in idiopathic scoliosis (Weiss and Werkmann, 1996; Rigo 1996, 1997, 1999a). Exercise is believed to improve the brace treatment of scoliosis by maintaining flexibility of the spine as well as preventing paraspinal muscle atrophy secondary to the immobilising effects of the brace.
2.4.4 SCOLIOSIS: 3D DEFORMITY
According to Dubousset (1992), from an anatomical point of view, a scoliotic deformity can be described as a series of vertebral segments placed in extension or lordosis, which deflect and axially rotate towards the same side. Lateral curve, anatomical lordosis and axial rotation are the three elements of a scoliotic lesion.
In all cases, the intention of bracing is to change the shape of the spinal column. The shape of a scoliotic spinal column is best defined from a geometric rather than an anatomical point of view. Aubin et al.,(1997) recently described scoliosis as a complex process of trunk deformation including morphological changes and a global transformation of the shape of the vertebral column, which moves from its original position in the sagittal plane, to a complex torsional geometry in the three dimensions of space.
The term torsion, has two meanings. One meaning is mechanical torsion, which refers to the torsional deformity of the spinal column being considered as a plastic structure and which includes an intravertebral torsion and an intervertebral torsion. In 50% of patients, intravertebral torsion is responsible for approximately 45% of total axial rotation (Aubin et al., 1997). For this reason, braces cannot correct this aspect as effectively as they correct the lateral curve. The term is also used as a geometrical or helicoidal torsion, which refers to the twisting of the spine considered as a line in space. The vertebral column, moved by deforming forces, changes its physiological shape in the coronal, transversal and sagittal planes, adopting extremely diverse anatomoradiological patterns.
2.5 CLASSIFICATION OF CURVE PATTERNS
Classification of curve patterns is necessary to allow comparisons and prognoses of various patients. In idiopathic scoliosis, the curve pattern generally does not change from that noted at the onset of the deformity. Although the sagittal plane X-ray is often evaluated for the identification of sagittal plane deformities, (i.e. hypokyphosis or hypolumbar and hyperlumbar lordosis), a scoliotic curve is classified by evaluation of the dorsal aspect of the coronal plane X-ray. Also, it is important to identify the direction of the curve or curves of the scoliosis pattern as a left or right. A left curve has the direction of the convexity to the left and its concavity on the right of the vertebral column. A right curve has the direction of the convexity to the right and its concavity on the left of the vertebral column. In all types of classification of scolioses patterns, the vertebral column is always viewed by its dorsal aspect or posterior view of the pelvis and vertebral column.
2.5.1 CLASSIFICATION OF COBB
Cobb (1948) reported the terms of major and minor curves, which are frequently used in the United States and United Kingdom. A major curve is more structural and deforming, whereas a minor curve is less structural and less deforming and is often called the compensatory curve. Cobb classified the following major and minor curves, which are helpful in outlining treatment and prognosis (Cobb, 1948):
- Single major high thoracic curve: A high thoracic curve with the apex in the upper thoracic spine, which may appear without a lower thoracic curve or with a small, flexible curve below.
- Single major thoracic curve: The apex lies within the thoracic spine, the upper end vertebra is between the 4th to 6th thoracic vertebra (T4 to T6), and the lower end vertebra is between the 11th thoracic to 2nd lumbar vertebras (T11 to L2). The majority of these curves are convex to the right and present hypokyphosis. This pattern is usually associated with a rotation prominence; the magnitude varies significantly from curve to curve and is not related to the degree of Cobb angle or to the rotation seen on the coronal plane radiograph.
- Single major thoracolumbar curve: This is a single curve with its upper end vertebra between T8 to T10 and the lower end vertebra at L3. The apical vertebra is T12 or L1. Both the upper thoracic and lower lumbar spine may show small compensatory curves, which are usually completely flexible.
- Single major lumbar curve: This is a lumbar curve, often small and flexible with the apex usually at L2. The upper end vertebra is between T11 to L1 and the lower end vertebra at L 4 or L5. A pelvic tilt is often present with this curve pattern.
- Major thoracic and minor lumbar curves: This curve pattern, which is commonly seen, consists of an upper curve with the upper end vertebra at T4 or T5 and the lower end vertebra at T12, and a lower curve has the upper end vertebra at T12 and the lower end vertebra L4 or L5. The upper curve is larger and more structural of the two.
- Double major thoracic and lumbar curves: This pattern consists of both thoracic and lumbar curves, both of which appear at the some time, usually during the juvenile years. Both curves are of nearly the same degree of Cobb angle and rigidity. The thoracic curve is generally convex to the right (but could be to the left) with the apical vertebra at T7 or T8, the upper end vertebra at T4, T5, or T6, and the lower end vertebra at T10, T11, or T12. The lower curve is generally convex to the left (but could be to the right), having its apical vertebra at L1 or L2 and extending to L4 or occasionally L5.
- Double major thoracic and thoracolumbar curves: The thoracic curve has its upper end vertebra at T4 and the lower end vertebra at T9 or T10, with its apex at T6 or T7. The convexity is usually to the right with minimal associated rib prominence. The thoracolumbar curve has its upper end vertebra at T9 or T10 and the lower end vertebra at L3, with an apex at the T12 – L1 disc space.
- Double major thoracic curves: This curve pattern is commonly presented as a left upper and right lower thoracic curves (however they could be to the right and left respectively). The upper curve has its upper end vertebra at T1 or T2 and the lower end vertebra at T5 or T6, with its apex at T3 or T4. The lower curve has its apex within the thoracic spine, with the upper end vertebra at T5 or T6 and the lower end vertebra between T 11 to L2.
- Multiple curve patterns: Multiple curves other than those described above do occur, but they tend to be short and nondeforming.
2.5.2 CLASSIFICATION OF CHÊNEAU
The classification used by Chêneau (1990, 1996a, 1996b) simplifies the patterns into two groups, 3-curve and 4-curve scoliosis, except for the rare exception of the “C” shaped scoliosis that can be found in spastic patients. Both the 3-curve and 4-curve patterns present two compensatory curves or half curves, one is located above and the other below the principal curve or curves of the coronal plane (Moe and Kettleson, 1970). Therefore a pattern with one primary curve with two compensatory curves is a 3-curve scoliosis and a pattern with two primary curves with two compensatory curves is a 4-curve scoliosis.
I) 3-CURVE PATTERN
This presents as a long thoracolumbar curve with the apex around T9 or T10, which is generally convex to the right (figure 2.2a). The thoracolumbar curve could be convex to the left, however it is more often to the right. To the opposite side of the thoracolumbar curve, cephalically there is a high thoracic (compensatory) hemi-curve with the apex around T1 to T4. To the opposite side of the thoracolumbar curve, caudally there is a low curve, which deviates and rotates the pelvis to the left. In the case that the thoracolumbar curve is to the left, the pelvis deviates and rotates to the right, (Chêneau, 1990, 1996a).
II) 4-CURVE PATTERN
This presents as two primary curves, one in the thoracic region and the other in the lumbar region (figure 2.2b). These double curves have two small compensatory curves or hemi-curves, one cephalic and the other caudal. The two compensatory curves or hemi-curves are not easily seen by viewing the pattern. The upper primary curve has a thoracic curve with the apex at T8 or T9 and the lower primary curve has a lumbar curve with the apex around L2. These double curves generally have the convexity of the thoracic curve to the right and the convexity of the lumbar curve to the left. The opposite curve direction could occur (i.e.: convex to the left in the thoracic region and convex to the right in the lumbar region); however it is less common.
To the opposite side of the thoracic curve, cephalically there is a high thoracic (compensatory) hemi-curve with the apex around T1 to T4. To the opposite side of the lumbar curve, caudally there is a low compensatory curve with the apex at L4, L5, or the 1st sacral vertebra (S1). The pelvis could be deviated to the right, not rotated or slightly rotated. (Chêneau, 1990, 1996a).
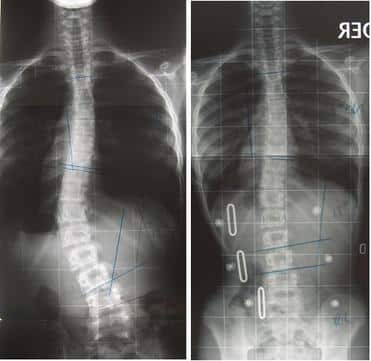
Figure 2.2 (a) Posterior view of a 3-curve scoliosis pattern, in this case , the thoracolumbar curve is convex to the right with the apex at T9 or T10, (represented as 2). The high thoracic (represented as 1) and low lumbosacral (represented as 3) curves are convex to the left with the apexes around T1 to T4 and L3 to S1 respectively. (b) Posterior view of a 4-curve scoliosis pattern, in this case , the thoracic (represented as 2) and lumbosacral (represented as 4) curves are convex to the right with the apexes around T7 to T9 and L2 or L3 respectively. The high thoracic (represented as 1) and low lumbar (represented as 3) curves are convex to the left with the apexes around T1 to T4 and L3 to S1 respectively.
|
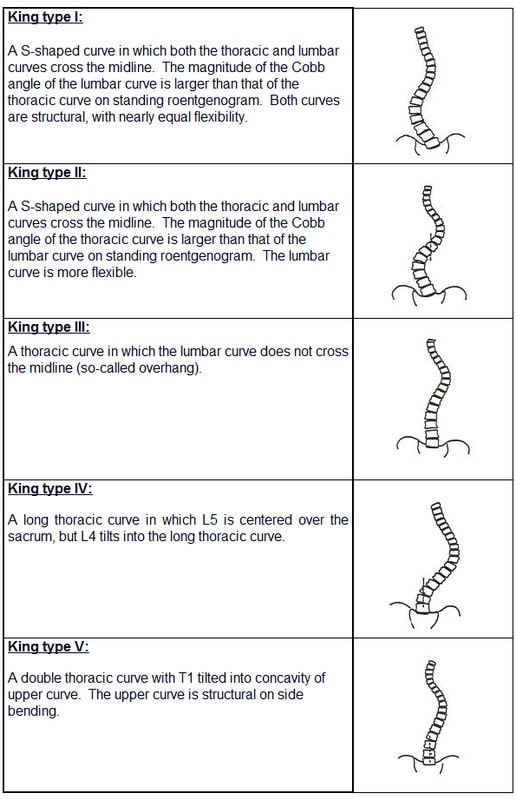
2.5.3 CLASSIFICATION OF KING 2.5.4 CLASSIFICATION OF CURVE RELATIONSHIP |
Results
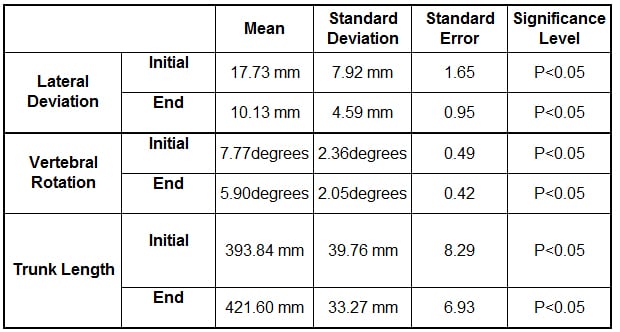
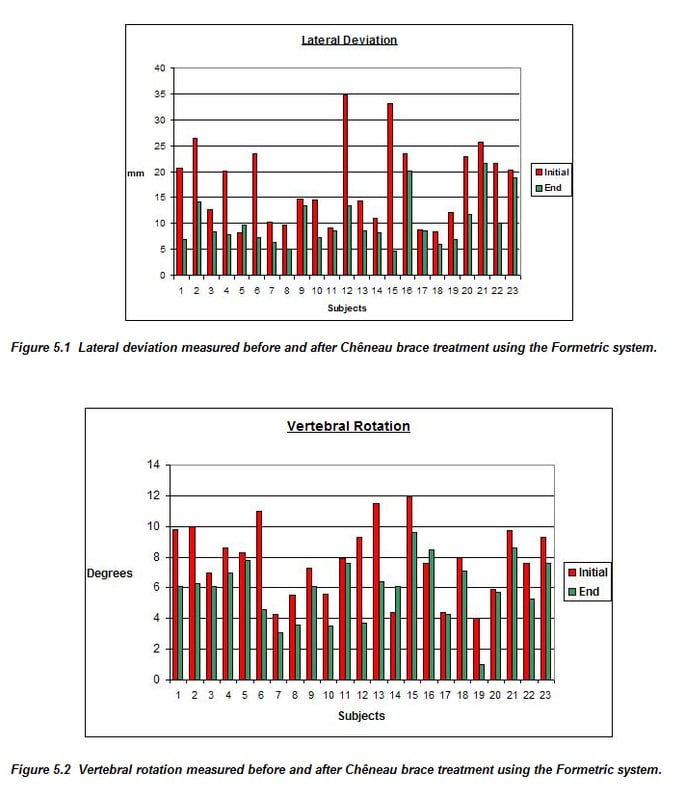
These data were analysed using a paired (dependent) t-test. There was a significant decrease in lateral deviation and rotation after Chêneau brace treatment. Also, there was a significant increase in trunk length.
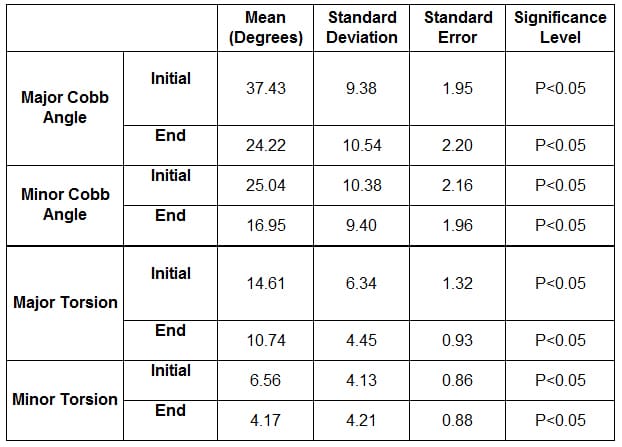
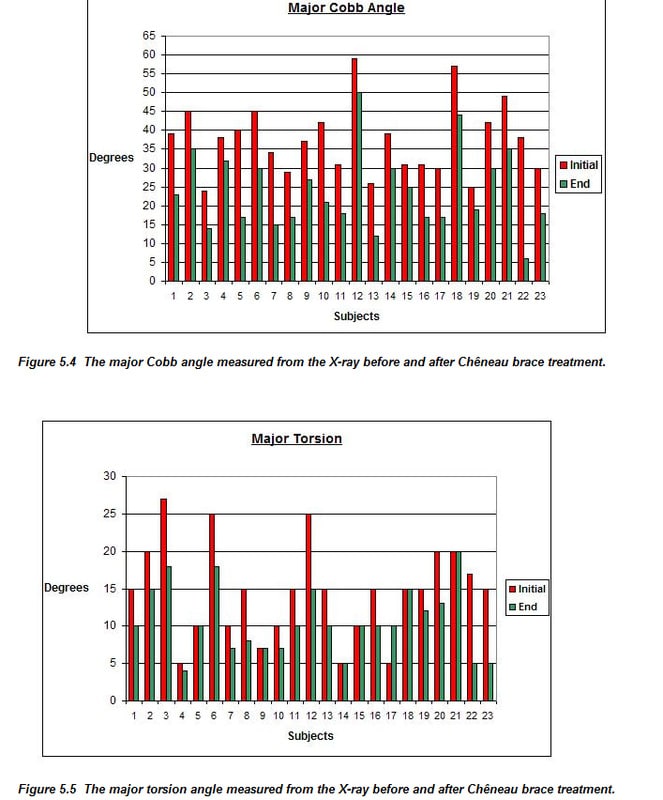
The major and minor curve and torsion angles for each subject were calculated using X-ray values (the Cobb and rotation angles respectively). The mean, standard deviation, standard error and significance level for each angle are shown in Table 5.2 for the 23 subjects.
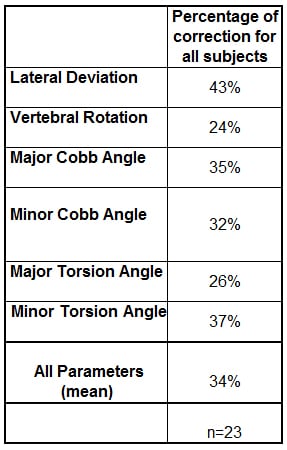
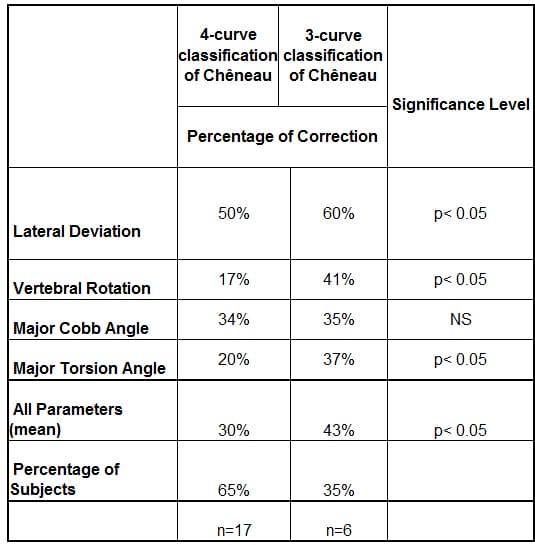
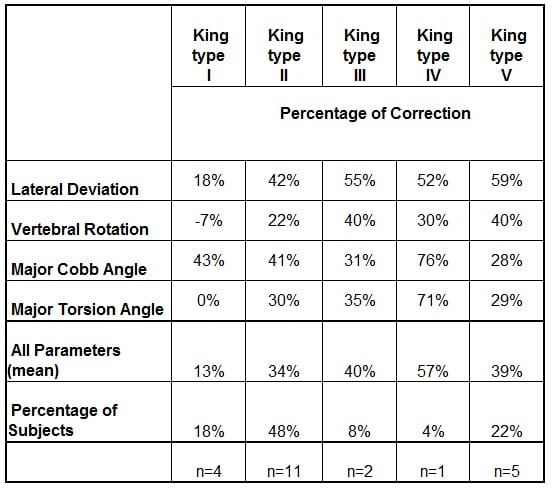
The percentage of correction was calculated for the subjects X-ray and topography values, also the total mean was calculated for all parameters, (table 5.3).
Figures 5.1 through 5.3 represent graphs of the descriptive statistics of the topography values using the Formetric system after scoliosis treatment with the Chêneau brace compared with before treatment (n=23).
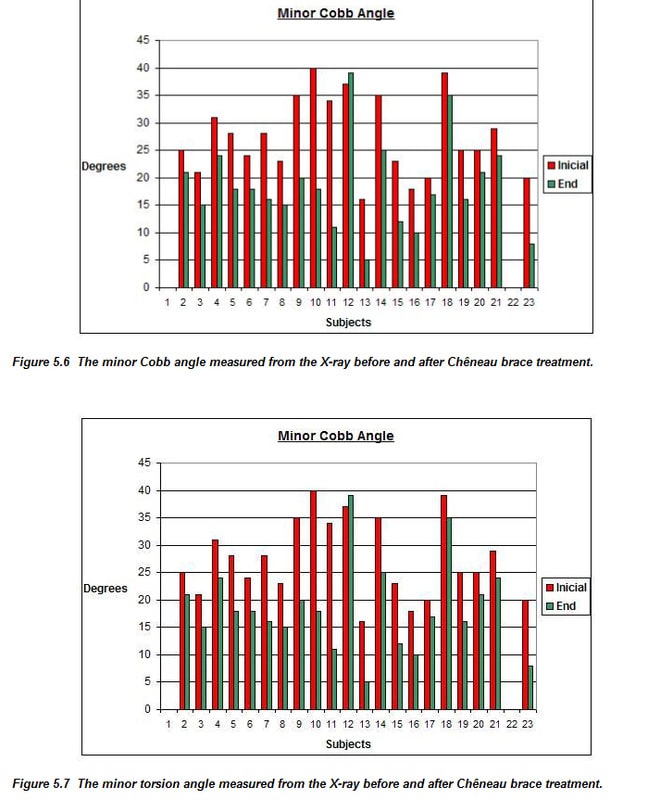
X-RAY VALUES
Figures 5.4 through 5.7 represent graphs of the descriptive statistics of the X-rays using the Cobb and torsion angles measured before and after scoliosis treatment with the Chêneau brace (n=23).
Discussion
COMPARISON OF TOPOGRAPHY VALUES
The results are consistent with the experimental hypothesis: those subjects who were treated during four years with the Chêneau brace would report at the end of treatment a reduction in lateral deviation and rotation compared with before the start of treatment. Also, there was a significant increase in the trunk length after four years of treatment compared with before the start of treatment. The paired (dependent) t-test results for lateral deviation, rotation and trunk length showed significant differences in topography values when using the Chêneau brace. When the subjects’ topographies were measured, the means were 17.73 mm and 10.13 mm before and after treatment respectively for the lateral deviation, 7.77 degrees and 5.90 degrees before and after treatment respectively for the rotation, and 393.84 mm and 421.60 mm before and after treatment respectively for the trunk length. The standard error in the experiment was small, hence it did not effect the results.
Perhaps the most reasonable explanations for these findings are concerned with the design of the Chêneau brace and the skeletal age of the subjects. The strategically placed pressure points with the large expansion rooms permit the correction of many aspects of the deformity. Maximum deflection is obtained by optimum location and shape-direction of the pressure points. The expansion areas of the brace allow small voluntary and involuntary movements as well as the patients own growth provides an active mechanism of correction. Also, in the thoracic region the expansion area has an additional advantage, in that the space was important for respiratory movement and for active correction in the direction of derotation and rekyphosis (reduction of flatback).
The lateral deviation results suggested that the Chêneau brace could correct curvature in the coronal plane. Conventionally, good scoliosis correction was considered when the vertebral column in the coronal plane, was as close as possible to vertical. However, the three-dimensional deformity of scoliosis needs to be evaluated and treated in all three anatomical planes. When more influence was put on the sagittal plane and rotation, the coronal plane deformity does not become less important, due to the coronal X-ray still being considered as standard good correction. There is support here for the experimental hypothesis. Furthermore, the placement of the pressure at the apex of the curve seems to play an important role. Chêneau (1996a) reported, that the curve pressure is placed two vertebras above and two vertebras below the apex of the thoracic curve and one vertebra above and one vertebra below the apex of the lumbar curve, therefore, maximal coronal plane correction is obtained.
The rotation results show that the Chêneau brace can correct the trunk rotation. Perhaps the most reasonable explanations for this finding were concerned with the three-dimensional design of the brace. The direction and location of the pressure points with their corresponding expansion chamber provides space for the correction of the rotation.
All the subjects in this study were measured by Rasterstereography and evaluated by means of surface reconstruction of the trunk utilising the Formetric system. Therefore less X-rays were required and a greater account of the three-dimensional aspects of scoliosis were taken into consideration when evaluating back shape. The use and effectiveness of the Formetric system for the evaluation of back shape has been reported by Weiss and Rigo (1994). However, Rigo (1999a) at present is the only author that has published work using the Formetric system to evaluate topography changes with treatment of the Chêneau brace. Rigo (1999a) presented at the meeting of the International Research Society of Spinal Deformities in Burlington, Vermont, that the Chêneau brace has significantly decreased the following topography parameters: trunk imbalance, lateral deviation and rotation. The results of this study were similar to those results found by Rigo (1999a), however, some of the subjects measured by Rigo (1999a) have been utilised in this experiment. Therefore, a direct comparison of this experiment with the study by Rigo (1999a) would be misleading. Consequently, there is no research to compare the consistency of these parameters, however, additional parameters have been evaluated in this experiment.
There was a significant change in trunk length after treatment when compared with before the start of treatment, this may seem obvious as these children would grow during their four years of Chêneau brace treatment. However, there seems to be a correlation between the growth and correction. For this reason, brace treatment is normally applied to the end of skeletal maturity because the body is normally more flexible and correctable during growth. After skeletal maturity the body is normally more rigid and as a result more difficult to correct.
The Risser sign (skeletal age) and magnitude of the curve play an important roll in evaluating the course of idiopathic scoliosis. The useful cross-correlation of incidence rates of progression of curves under 29 degrees was reported by Lonstein et al., (1995). The two factors considered were the curve magnitude and maturity as assessed by the Risser sign (table 2.2). These figures are used to record the natural history and incidence of progression when evaluating the effectiveness of treatment.
For curves of 20 to 29 degrees in an immature child with a Risser sign of 0 or 1, the incidence of progression was 68 %. On the other extreme, for curves under 19 degrees in a mature adolescent with a Risser sign of 2 or more, the incidence of progression was 1.6%. In the other two groups, that is, smaller curve (less than19 degrees) in an immature child (Risser 0 or 1), and larger curve (20 to 29 degrees) in a mature child (Risser 2 or more), the incidence of progression is approximately the same at 22 to 23% (Lonstein et al., 1995).
The subjects in this study who have Risser 0 and Risser 1 were 61% and 26% respectively, and 37.43 degree Cobb angle means, therefore the incidence of progression, if untreated was at least 68%. This was assuming that greater than 30 degree curves would have a greater progression percentage than that of curve less than 30 degrees. However, the possibility of correction in these low Risser subjects was worse as they had a higher growth potential compared to Risser 3 or 4. There is a significant reduction between before and after topography values. Therefore, when these topography values are compared with the incidence of progression, it could be assumed that the Chêneau brace has significantly changed the prognosis of the subjects in this study.
It is possible that the treatment time was insufficient to differentiate the long term effect of the orthotic treatment. However, considering that long term idiopathic scoliosis treatment should be continued until the completion of skeletal growth, approximately 18 years of age in girls, with the average follow-up time of 2 years, the difficulties in scoliosis research could be understood.
There is support here for the experimental hypothesis, however, the subjects were additionally provided with physiotherapy treatment. Unfortunately, it is not possible to assess the extent of physiotherapy, as this experiment failed to explore this question. Future work should therefore check on this possibility, and additionally evaluate the effects of Chêneau brace treatment with and without physiotherapy. Nevertheless, Weiss and Werkmann (1996) have reported the favourable values of physiotherapy in scoliotic patients, and Rigo (1999a, 1999b) claims this could improve the actions of the Chêneau brace by making the curve more flexible and preventing muscle atrophy.
6.2 MAJOR AND MINOR COBB ANGLE VALUES
The results are consistent with the experimental hypothesis: that the Chêneau brace would prevent the progression of the major and minor Cobb angles. The paired (dependent) t-test results for major and minor Cobb angles showed significant reductions when using the Chêneau brace. When the subject’s X-ray values were measured, the means were 37.43 degrees and 24.22 degrees before and after treatment respectively for the major Cobb angles as well as 25.04 degrees and 16.95 degrees before and after treatment respectively for the minor Cobb angles. The standard error in the experiment was small, hence it did not affect the results.
6.3 MAJOR AND MINOR TORSION VALUES
The results are consistent with the experimental hypothesis: that the Chêneau brace would prevent the progression of the major and minor torsion angles. The paired (dependent) t-test results for major and minor torsion angles showed significant reductions when using the Chêneau brace. When the subject’s X-ray values were measured, the means were 14.61 degrees and 10.74 degrees before and after treatment respectively for the major torsion angles as well as 6.56 degrees and 4.17 degrees before and after treatment respectively for the minor torsion angles. The standard error in the experiment was small, hence it did not affect the results.
Perhaps the most reasonable explanations for these findings are concerned with the design of the Chêneau brace. The strategically placed pressure points with large expansion rooms allow for correction of many aspects of the deformity. Maximum deflection is obtained by optimal location and shape-direction of the pressure points. The expansion areas of the brace permit small voluntary and involuntary movements, as well as the patients own growth providing an active mechanism of correction. Also in the thoracic region the expansion area has another advantage, in that the space is important for respiratory movement, which provides active correction in the direction of derotation and rekyphosis.
6.4 COMPARISON OF COBB ANGLE MAGNITUDE AND RISSER SIGN
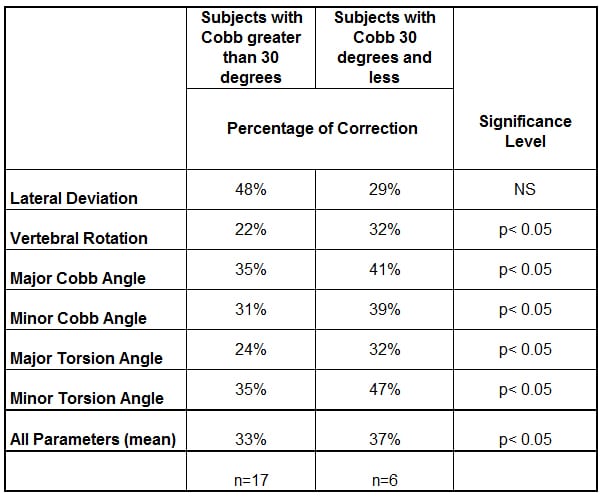
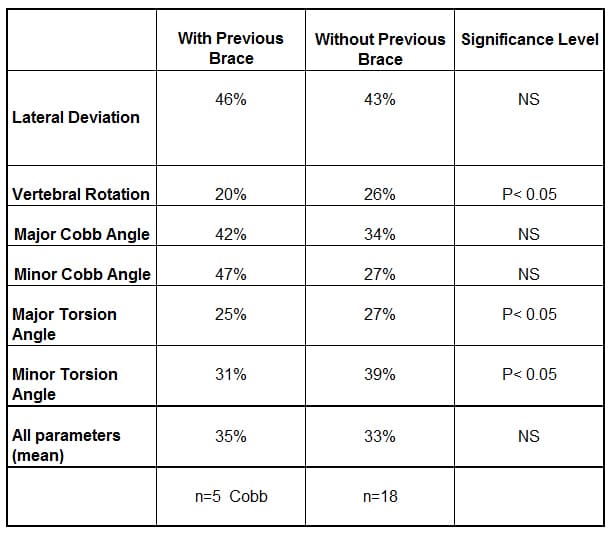
The results are consistent with the experimental hypothesis: those subjects who had a Cobb angle 30 degrees or less would report a significant correction of the scoliotic deformity compared to those subjects who had a Cobb angle greater than 30 degrees.
The paired (dependent) t-test results for vertebral rotation, major Cobb angle, minor Cobb angle, major torsion angle and minor torsion angle showed significant differences in subjects who had a Cobb angle 30 degrees or less compared to subjects who had a Cobb angle greater than 30 degrees when using the Chêneau brace. The subjects who had a Cobb angle 30 degrees or less had no significant improvement of correction of the lateral deviation compared to subjects who had a Cobb angle greater than 30 degrees when using the Chêneau brace. However, a significant correction of the scoliotic deformity, which refers to the parameters, lateral deviation, vertebral rotation, major and minor Cobb angles as well as major and minor torsion angles, found a significant difference when analysed as a group.
Studies of the natural history of untreated scoliosis have presented a clear indication that scoliotic curves with Cobb angles greater than 30 degrees show a significant increase in progression compared to Cobb angles less than 30 degrees (Clarisse, 1974, Fustier, 1980, Lonstein and Carlson, 1984, Bunnell, 1986,). Therefore in this study, it was assumed that subjects with Cobb angles less than 30 degrees would produce a better correction compared to subjects with Cobb angles 30 degrees or greater. Although, this study shows a significant difference in all parameters, the roll of natural history was evaluated in subjects who used the Chêneau brace. This was done by accepting the hypothesis that the Chêneau brace had a significant effect on the scoliosis. However the natural history of untreated scoliosis also facilitated good results in subjects with less than 30 degrees Cobb angles because in this group of patients, there was a percentage of subjects that had a favourable natural history. This implies that the group of subject with less than 30 degrees Cobb angle obtained superior correction due to not only the positive effects of the Chêneau brace, but also because the natural history shows in general less progression. Also, generally larger curves are more rigid compared to smaller curves and therefore they are more difficult to correct. The opposite occurs with smaller curves as they are more flexible and therefore normally have better correction.
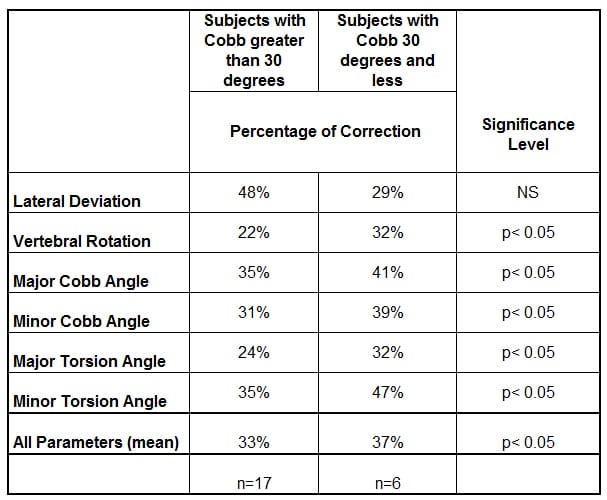
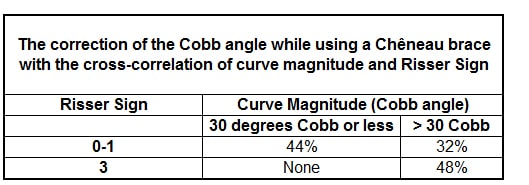
The correction of the Cobb angle while using a Chêneau brace with the cross-correlation of curve magnitude and Risser sign showed that subjects with Cobb angles less than 30 degrees and low Risser signs (Risser signs 0 and 1) had a greater percentage of Cobb angle correction (44%) compared with subjects with Cobb angles greater than 30 degrees and low Risser signs (Risser signs 0 and 1), which had 32% of Cobb angle correction.
Also, the correction of the Cobb angle while using a Chêneau brace with the cross-correlation of curve magnitude and Risser sign showed that subjects with Cobb angles greater than 30 degrees and high Risser signs (i.e.: Risser signs 3) had a greater percentage of Cobb angle correction (48%) compared with subjects with Cobb angles greater than 30 degrees and low Risser signs (Risser signs 0 and 1), which had 32% of Cobb angle correction.
Therefore, the results of this study demonstrate that subjects with lower Risser signs (i.e. the greater the growth potential) presented less Cobb angle correction compared to subjects with higher Risser signs (i.e. less growth potential). These results correspond with those reported by Goldberg et al., (1993); Lonstein et al., (1995); Peterson and Nachemson, (1995), which claim that when analysing the growth potential and curve progression, it is generally true that the younger the child (i.e. the greater the growth potential), the greater the incidence of progression if untreated. Hence, this also was true for subjects who were treated with the Chêneau brace, in which the younger the child, the greater possibility of less correction compared to an older child.
Although Dickson (1984) claimed that there is no evidence which demonstrates conclusively that wearing a spinal brace affects the natural history of scoliosis, this study demonstrates that the Chêneau brace was effective in changing the natural history of progressive scoliosis. This was evaluated in the cross-correlation of curve magnitude and Risser sign, which showed that although the Chêneau brace significantly corrected the parameter of the subject, the natural history of scoliosis could have improved the results in subjects with higher Risser signs (i.e. Risser sign 3) and lower Cobb angles (i.e. less than 30 degrees). However, 85% and 65% of the subjects in this study had Risser signs 0 or 1 and Cobb angles greater than 30 degrees respectively. As a result, it was valued by using the cross-correlation by Lonstein (1995), of curve magnitude and Risser sign that the majority of these subjects had approximately 68% possibility of curve progression if left untreated. Nevertheless, this study reported a statistically significant difference in all parameters, therefore correction and not progression was effectively obtained.
This study showed significant differences in all parameters (except lateral deviation) for subjects who had a 30 degrees Cobb angle or less compared to subjects who had greater than 30 degrees Cobb angle when using the Chêneau brace. However it was interesting to observe that the subjects who presented greater than 30 degrees Cobb angle had significantly better correction of lateral deviation (48% correction) compared to those subjects who had less than 30 degrees Cobb angle (29% correction). This phenomenon was first noted by Rigo (2000), it was stated that Cobb angles with larger magnitudes produced greater changes in lateral deviation. This was because not all the forces produced by the Chêneau brace could produce changes in the vertebral column, however these forces were capable of causing greater changes to the trunk shape, in which the increased correction of lateral deviation was obtained. Therefore, the greater the Cobb angle, the greater the lateral deviation, which allows a greater percentage of correction of the trunk deformities.
The Cobb angle results of previous Chêneau brace studies (Hopf and Heine, 1985, Liljenqvist et al., 1998) were slightly better than this study, however, this could be attributed to the fact that their subjects had lower initial Cobb angles. Hence, a greater probability of an increased Cobb angle correction.
This study presented better results than the studies presented by Rigo (1999a, 1999b) in all of the following parameters, lateral deviation, vertebral rotation, major Cobb angle, minor Cobb angle, major torsion angle and minor torsion angle. However, approximately 11 subjects from that study were also utilised in this study. Also the studies by Rigo (1999a, 1999b) reported 49 and 105 subjects respectively, therefore it is difficult to compare this study with those studies presented by Rigo (1999a, 1999b). Nevertheless, it was observed that the study presented by Rigo (1999a, 1999b), had a significant number of subjects who had previous brace treatment. Rigo (1999a, 1999b) claimed that this could have affected the end result, due to the spinal rigidity produced by the previous failed brace treatments from other clinics.
6.5 COMPARISON OF PREVIOUS BRACE WEARERS
The results are not consistent with the experimental hypothesis: those subjects who had no previous brace treatment would report a significant correction of all parameters of the scoliotic deformity compared to those subjects who had previous brace treatment. The paired (dependent) t-test results showed no significant differences in subjects who had previous brace treatment compared to subjects who had no previous brace treatment when using the Chêneau brace.
Although Rigo (1999a, 1999b) claimed that his study had subjects with rigid curve due to poor previous brace treatment, this study found no significant difference in the group who had previous brace treatment. Generally in Spain, patients who go to a private clinic (Instituto Elena Salva) from another clinic (national health service or private) would be because they were not satisfied and had poor results from the previous brace treatment. It was assumed that the failed treatment produced a larger curve and therefore more rigid vertebral column. However this study found no significant difference in the subject who had previous brace treatment compared to those who had no previous brace treatment. This implies that the poor previous brace treatment was due to poor previous brace type and design, as a result these subjects were capable of obtaining a significant correction of all parameters. The brace type and design plays an important roll in the individual patient results, however the Chêneau brace evaluation, design and rectification processes were very complicated and required a great amount of time.
6.6 INTERPRETATION AND IMPLICATIONS OF THE CLASSIFICATION OF CHÊNEAU AND THE CLASSIFICATION OF KING PATTERNS
There was a significant difference of the percentage of correction of the 3-curve scoliosis compared to the 4-curve scoliosis pattern. This implies that the Chêneau brace system was more effective for 3-curve patterns compared to 4-curve patterns. These results agree with Lonstein (1995), who reported that double-curve pattern (which could be considered as a 4-curve pattern) had a greater possibility of progression compared to single curves (which could be considered as a 3-curve pattern). Therefore, these results show that the Chêneau brace had a significant effect on the scoliotic deformity (all parameters), however the subjects with 3-curve scoliosis patterns reported better results than the 4-curve scoliosis patterns.
The King type III, King type IV and King type V curve patterns presented a higher percentage of correction compared with King type I and King type II curve patterns. The King type III, King type IV and King type V patterns could be considered as 3-curve scoliosis and the King type I and King type II could be considered as 4-curve scoliosis (Chêneau, 1996a, Rigo, 1997). Therefore these results show a relationship between King type III, IV and V to 3-curve patterns, also, King type I, and II patterns to 4-curve patterns. As a result, when grouped together they both show 3-curve and King type III, IV and V had greater percentage of correction compared to 4-curve or King type I and II pattern.
The Cobb angle results show that the Chêneau brace can prevent progression of the coronal plane curvature. Due to the introduction of X-rays, the coronal plane radiographic view has become the standard for the evaluation of the severity of scoliosis. Therefore, conventionally, good scoliosis correction was considered when the vertebral column, was as close as possible to vertical in the coronal plane and the Cobb angle was as close as possible to 0 degrees. Although the rotation is often measured in the coronal plane X-ray and the sagittal plane X-ray is sometimes taken, this still falls short of a three-dimensional evaluation and correction.
The three-dimensional deformity of scoliosis should be evaluated and treated in all three anatomical planes (Winter et al., 1975; Dubousset 1992; Chêneau, 1990, 1996a, 1996b; Rigo and Chêneau, 1997; Aubin et al., 1997; Wood and Rigo, 1999). As a result, the Cobb angle measurement is insufficient to optimally assess and evaluate idiopathic scoliosis.
The good coronal plane results that are often reported by conventional TLSOs (Boston, Malaga, Lyon) and casting braces appear at first sight to be positive with a good correction of the deformity. However, this could be a major mistake when considering the three-dimensional model. Aubin et al., (1997) have claimed that the Boston brace produces a lordotic effect in the thoracic region. The normal physiological curve in the thoracic region is kyphotic and therefore this has a negative effect, which occurs in all of the conventional TLSOs, as their upper shapes are very similar.
Generally, bracing theories consider three different thoracic pad locations. The most common location is utilised in the Lyon and Malaga braces. In these braces the thoracic pressure pad is placed covering the entire length of the curve, with the width extending from approximately the lateral midline to the vertebra (posterior midline). The Boston brace thoracic pad is located below the apex of the curve with the width being similar in the Malaga and Lyon braces. However, the most different thoracic pressure is in the Chêneau brace, which normally does not use pads, but instead relies on direct contact of the thermoplastic brace against the patient. This provides a smoother surface for deflexion and derotation (Chêneau et al., 1997). The location is also different, with the pressure being two vertebras above and two below the apex of the curve and the width extending from the lateral midline to approximately 60% of the distance between the lateral midline and the posterior midline. This is much less than the previous braces. Also the direction of the forces are more oblique than in conventional braces with pads that are more laterally and anteriorly directed. This shorter width leaves space for derotation and deflexion of the trunk, also the alignment of these forces facilitates these actions. Therefore, as the thoracic curve is reduced, more of the patient’s back becomes in contact with the brace.
These theories of the Chêneau brace pressure placement and direction seem to produce a reduction of the Cobb angle in patients with idiopathic scoliosis. However the effect of each component is difficult to measure due to the numerous amounts of variables in a scoliosis deformity. Therefore, the effectiveness of the pressure pad placement and direction can be measured as a whole using the Cobb angle. However, caution must be applied when using only the Cobb angle, as a decrease in the Cobb angle with increase of hypokyphosis would not be the objective of the three-dimensional correction outlined by Dubousset (1992).
Similar theories are applied by the Boston, Lyon and Malaga braces for the lumbar curve pressure pad placement and direction of forces. The pads of the Malaga and Lyon braces are the same shape, covering the entire curve and extending from the lateral midline to just before the posterior midline. The Boston brace again places that pressure pad just below the apex of the curve and extends from lateral midline to just before the posterior midline. The Chêneau brace applies pressure that is located one vertebra above and one vertebra below the apex of the curve and is applied directly to the patient via the plastic brace. The pressure comes from the ventral aspect of the brace and extends between 25% from the posterior midline to crossing over the posterior midline, depending on the lumbar lordosis of the patient. Therefore, it can be seen that the Chêneau brace has taken into consideration the sagittal plane deformity as well as the pelvis rotation.
These results are consistent with those of Chêneau (1990), Hopf and Heine (1985), as well as Liljenqivist et al., (1998). However, the results of Chêneau (1990), and Hopf and Heine (1985), are from the Chêneau brace model 1992, therefore, due to the substantial changes in the current design, it would be difficult to compare the 1992 model with the present one. The Cobb angle results of the Chêneau brace could be compared with long term result of Milwaukee brace andBoston brace (Carr et al., 1980; Emans et al., 1986), however these early studies were only a single plane study and therefore are insufficient when compared to the three-dimensional Chêneau brace. Also, these studies evaluated the percentage of initial Cobb angle correction of the brace, as well as to the end of brace treatment. Whereas this study could not evaluate all the subjects’ initial correction because many of them were previously treated patients, who came from other clinics with failed brace treatment. As a result, many of the patients in this study had initial corrections that were measured using a brace other than the Chêneau brace.
Based on these observations, future research on the Chêneau brace would include a larger sample, measured from start of treatment, until two years after treatment has finished, and a group of subjects that have had no previous brace treatment.
Also, the initial correction of scoliosis when wearing the Chêneau brace could be compared to that of the Boston,Milwaukee and Lyon braces. Further investigation is then warranted to analyse sagittal plane X-ray values to evaluate the long term effect of the Chêneau brace in hypokyphosis.
Thesis Conclusion
The present experiment focused on the topography and X-ray measurements of idiopathic scoliosis subjects before and after treatment with the Chêneau Brace. The results are based on a sample size of 23 subjects during a four-year period, and thus the following conclusions appeared to be warranted:
1. The Chêneau brace significantly decreases lateral deviation and rotation in idiopathic scoliosis patients.
2. The Chêneau brace significantly decreases major and minor Cobb and torsion angles in idiopathic scoliosis patients.
3. Subjects with greater than 30 degrees Cobb angle and a Risser sign 0 or 1 had significantly less correction compared to those subjects with less than 30 degrees Cobb angle and Risser sign 0 or 1 and those with greater than 30 degrees Cobb angle and Risser sign 3.
4. The Chêneau brace significantly improved all parameters in idiopathic scoliosis subjects who had previous brace treatment as well as those who had no previous brace treatment.
5. The Chêneau brace significantly improved idiopathic scoliosis in subjects who presented King type III, IV and V or 3-curve scoliosis patterns compared to King type I and II or 4-curve scoliosis patterns.
In this study, significant reductions in topography and X-ray values were found in these idiopathic scoliosis subjects, this was due to the superior design and functional characteristics which allowed improved detorsion and sagittal normalisation, which would effect correction of the coronal plane, resulting in some elongation of the spine, without any significant distraction force.
The Chêneau brace has valid principles that facilitate a 3D correction of idiopathic scoliosis, with strong emphasis on the sagittal plane configuration, as well as the treatment of all aspects of the deformity. The technical difficulties as well as the fitting and rectification time involved in the manufacture of the brace have limited its use to specialised clinics. However, for optimal three-dimensional treatment, the difficulties are valued. As the negative sagittal plane effects are often produced by the standard TLSOs, a greater need for the Chêneau brace is required.
Further investigation is then warranted to analyse sagittal plane X-ray values to evaluate the long term effect of the Chêneau brace in hypokyphosis. Also, ideally the initial correction of scoliosis when wearing the Chêneau brace should be compared to that of the Boston, Milwaukee and Lyon braces using identical experimental techniques.
The standard brace system that treats progressive scoliosis by a “sandwich effect” may obtain modest results in the coronal plane, however, they often neglect the sagittal and transversal planes. The three-dimensional deformity of scoliosis requires a three-dimensional brace design when considering nonoperative treatment. Therefore, the hypercorrection Chêneau brace system facilitated by the Rigo brace design would play an important roll in this treatment. It could be seen that daily practice with the Chêneau brace must be performed in conjunction with other effective areas of treatment, such as patient evaluation, curve classification, brace design and fitting, so as to optimise the treatment regime for the patient.
References
1. Abbott, E.G. (1912) Correction of lateral curvature of the spine. Journal of Medicine, 17, pp 835-846.
2. Abbott-Byrd, J. (1988) Current theories on the etiology of idiopathic scoliosis. Clinic Orthopedic, 229, pp114-119.
3. Adams, (1849) The genuine works of Hippocrates, Translated by Francis Adams. J W. Edwards, New York.
4. Aksenovich, T. I., Semenov, I.R., Ginzburg, E.K., Zaidman, A.M. (1988) Preliminary analysis of inheritance of scoliosis. Genetika, 24, pp 2056-2063.
5. Aubin, C.E., Dansereau, J., De Guise, J.A., Labelle, H. (1996) A study of biomechanical coupling between spine and rib cage in the treatment by orthosis of scoliosis. Ann Chir,50, pp 641-650.
6. Aubin, C.E., Dansereau, J., De Guise, J.A., Labelle, H. (1997) Rib cage-spine coupling patterns involved in brace treatment of adolescent idiopathic scoliosis. Spine, 22, pp 629-635.
7. Blount, W.P., Schmidt, A.C., Kelver, E.D. (1958) Milwaukee brace in the operative treatment of scoliosis. Journal of Bone of Joint Surgery, 40, p 511.
8. Blount, W.P., MOE, T.H. (1980) The Milwaukee Brace, 2nd ed. Williams and Wilkins, Baltimore.
9. Brooks, H.L., Azen, S.P., Gerberg, E. et al. (1975) Scoliosis: a prospective epidemiological study. Journal of Joint and Bone Surgery, 57A, pp 968-972.
10. Bunnell, W.P. (1986) A study of the natural history of idiopathic scoliosis. Spine, 11, pp 773-776.
11. Bunnell, W.P. (1988) The natural history of idiopathic scoliosis. Clinical orthopaedics,229, pp 20-25.
12. Butterworth, T.R., James, C. (1969) Electromyographic studies in idiopathic scoliosis.South Medicine Journal, 62, pp 1008-1010.
13. Cahuzac, J.P., Sales de Gauzy, J., Kany, J. (1993) Traitement de 161 scolioses idiopatiquepar le corset de C.T.M. In: Institut Cátala de la Salut (ed.), En libro de comunicaciones del 2º Congreso, Transpirenaico de Rehabilitación Ciutat Sanitària i Universitaria de Ballvitge. L’Hospitalet, Barcelona.
14. Carr, W.A., Moe, J.H., Winter, R.B., Lonstein, J.E. (1980) Treatment of idiopathic scoliosis in the Milwaukee brace. Journal of Bone and Joint Surgery, 62, pp 599-612.
15. Chase, A., Pearcy, M., Bader, D. (1993) Spinal orthosis. In: Wallace, W.A. (ed.), Biomechanical basis of orthotic management. Butterworth-Heinemann, Oxford, pp 234-251.
16. Chêneau, J. (1990) Orthese de scoliose, 1st edition. Chêneau, J., Saint Orens.
17. Chêneau, J. (1994) Corset-Chêneau. Manuel d´ortopedic des scolioses suivant la technique originale. Frison-Roche, Paris.
18. Chêneau, J. (1996a) Orthese de scoliose, 2nd edition. Chêneau, J., Saint Orens.
19. Chêneau, J. (1996b) Corsé corrector de escoliosis; principios y perspectivas. Técnica Ortopédica Internacional, 36, pp 123-132.
20. Chêneau, J., Rigo, M., García, J. (1997) 1st Workshop on the theory and practical aspects of the Chêneau brace. Instituto de Especialidades Ortopédicas, Sevilla.
21. Child, A., Aubry, M., Brice, G., Park, E., Putnam, E., Milewicz, D. (1999) The role of fibrillin 1 and fibrillin 2 in severe scoliosis. In: Stokes (ed.), Research into Spinal Deformities 2. Studies in Health, Technology and Informatics. IOS Press. Amsterdam, pp 213-215.
22. Clarisse, P. (1974) Prognostic evolutif des scolioses idiopathiques mineures de 10 degrees to 29 degrees en periode de croissance. Univ Claude Bernard, Doctoral thesis, Lyon.
23. Cobb, J. (1948) Instruction course lecture-outline for study of scoliosis. American Academy of Orthopaedic Surgeons, 5, pp 23-36.
24. Cowell, H.R., Hall, J.N., MacEwen, G.D. (1969) Familial patterns of idiopathic scoliosis.Clinical Orthopaedics, 86, pp 121-131.
25.Czeizel, A., Bellyei, A., Barta, O., Magda, T., Molnar, L. (1978) Genetics of adolescent idiopathic scoliosis. J Med Genet, 15, pp 424-427.
26. Dickson, R.A., Stamper, P., Sharp, A.M., Harker, P., (1980) School screening for scoliosis: cohort study of clinical trial. Acta Orthop Scand, 49, pp 46-48.
27. Dickson, R.A. (1984) The pathogenesis of idiopathic scoliosis. Journal of Bone and Joint Surgery, 66, pp 8-15.
28. Drummond, D.S., Gauagni, J., Keene, L.S. (1984) Interspinous process wiring for idiopathic scoliosis. Paediatric Orthopaedics, 9, pp 541-550.
29. Drerup, B., Hierholzer, E. (1994) Back shape measurement using videoresterstereography and three-dimensional reconstruction of the spinal shape. Clin Biomech, 9, pp 28-36.
30. Dubousset, J. (1992) Importance of the three-dimensional concept in the treatment of scoliotic deformities. In: Dansereau, J. (ed.), International Symposium on 3D Scoliotic Deformities joined with the 7th International Symposium on Spinal Deformity and Surface Topography. Gustav Fischer Verlag, Ed, Germany, pp 302-311.
31. Duval-Beaupere, G. (1970) Pathogenic relationship between scoliosis and growth. In: Zorab, P. A. (ed.), Scoliosis and Growth, Proceedings of a Third Symposium. Churchill Livingstone, Edinburgh, pp 58-64.
32. Duval-Beaupere, G., Taussig, G., Mouilleseaux, B., Pries, P., Mounier, C. (1992) Prognostic factors for idiopathic scoliosis. In: Dansereau, J. (ed), International Symposium on 3D Scoliotic Deformities. Gustav Fischer Verlag, Ed Germany, pp 211-216.
33. Edgar, M.A., Chapman, R.H., Glasgow, M.M. (1982) Preoperative correction in adolescent idiopathic scoliosis. Journal of Bone and Joint Surgery, 56b, pp 530-535.
34. Edmondson, A.S., Morris, J.T. (1977) Follow-up study of Milwaukee brace treatment in patients with idiopathic scoliosis. Clinic Orthopaedic, 126, pp 58-61.
35. Emans, J.B., Kaelin, A., Bancel, P., Hall, J.E., Miller, M.E. (1986) The Boston bracing system for idiopathic scoliosis. Follow-up results in 295 patients. Spine, 11, pp 792-801.
36. Fillio, N.O., Thompson, M.W. (1971) Genetic studies in scoliosis. Proceedings of the Scoliosis Research Society. Journal of Joint and Bone Surgery, 53A, p 199.
37. Fustier, J. (1980) Evolution radiologique spontanee des scolioses idiopathiques de moins de 45 degrees en periode de croissance. Etude graphique retrospective de cente dossier due Centre d¨adaptation fanctionnelle de massues. Thesis, Universite Claude-Bernard, Lyon.
38. Giorgi, S., Martucci, G., Losito, A., Cinnella, P., Caforio, G. (1996) El corsé Chêneau en el tratamiento de la escoliosis idiopática. Principios biomecánicos y realización técnica.Técnica Ortopédica Internacional, 33, pp 17-22.
39. Goldberg, C.J., Dowling, F.E., Hall, J.E., Emans, J.B. (1993) A statistical comparison between natural history of idiopathic scoliosis and brace treatment in skeletally immature adolescent girls. Spine, 18 , pp 902-908.
40. Henssge. J, (1967) Electromyographischer Beitrag sum Skoliosen-problem. Fortschr Med, 82, pp 665-668.
41. Herman, R., Maulucci, R., Stuyck, J. et al. (1979) Vestibular functioning in idiopathic scoliosis. Orthop Trans, 3, p 218.
42. Hidalgo, A.H. (1993) Nueva aportación del corsé de Málaga al pronóstico y tratamiento de la escoliosis. Ph.D. Thesis, Universidad de Sevilla, Sevilla.
43. Hopf, C., Heine, J. (1985) Long-term results of the conservative treatment of scoliosis using the Chêneau brace. Z Orthop Ihre Grenzgeb, 123, pp 312-322.
44.Huebert, H.T. (1967) Scoliosis: A brief history. Manitoba Medical Review, 11, pp 452-456.
45. Katz, D.E., Richards, B.S., Browne, R.H., Herring, J.A. (1997) A comparison between the Boston brace and the Charleston bending brace in adolescent idiopathic scoliosis. Spine,12, pp 1302-1312.
46. Kehl, D.K., Morrissy, R.T. (1988) Brace treatment in adolescent idiopathic Scoliosis.Clinical Orthopaedics, 229, pp 37-43.
47. King, H.A., Moe, J.H., Bradford, D.S., Winter, R.B. (1983) The selection of fusion levels in thoracic idiopathic scoliosis. Journal of Bone and Joint Surgery, 65, pp 1302-1303.
48. Kotwicki, T., Marciniak, W., Pietrzak, S. (1999) The immediate 3D effect of the Chêneau Brace on thoracolumbar scoliosis. Société Internationale de Recherche et d’Etude sur le Rachis (S.I.R.E.R.), 24, p 35.
49. Labelle, H., Dansereau, J., Bellefleur, C., Poitras, B. (1995) Comparison between preoperative and postoperative three-dimensional reconstructions of idiopathic scoliosis with the Cotrel-Dubousset procedure. Spine, 20, pp 87-92.
50. Labelle, H., Dansereau, J., Bellefleur, C., Poitras, B. (1996) Three-dimensional effect of the Boston brace on the thoracic spine and rib cage. Spine, 21, pp 59-64.
51. Legaye, J., Orban, C. (1995) Evolution of scoliosis by Optical Scanner I.S.I.S. In: D’Amico M., Merolli A., Santambrogio G.C. (ed.) Threedimensional Analysis of Spinal Deformities, IOS Press, Amsterdam.
52. Lenke, L.G., Bridwell, K.H., O’Brien, M.F., Baldus, C., Blanke, K. (1994) Recognition and treatment of the proximal thoracic curve in adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation. Spine, 19, pp 1589-1597.
53. Lenke, L.G., Betz, R.R., Bridwell, K.H., Clements, D.H., Harms, J., Lowe, T.G., Shufflebarger, H.L. (1998) Intraobserver and interobserver reliability of the classification of thoracic adolescent idiopathic scoliosis. Journal of Bone and Joint Surgery, 80, pp 1097-1106.
54. Lihvar, G.T., Putilova, A.A., Tabin, V.I. (1975) Statistical and correlation analysis of Electrical muscle activity in congenital scoliosis. Orthop Travmatol Protez, 36, pp 9-14.
55. Liljenqvist, U., Niemeyer, T., Grävinghoff, T., Halm, H. (1998) Conservative treatment of idiopathic scoliosis with the Chêneau brace. In: Proceedings book of the annual meeting of the European Spine Society combined with the European Spinal Deformity Society, Zurich.
56. Lonstein, J.E., Bjorklund, S., Wanninger, M.H., Nelson, R.P. (1982) Voluntary school screening for scoliosis in Minnesota. Journal of Joint and Bone Surgery 64A, pp 481-488.
57.Lonstein, J.E., Carlson, J.M. (1984) The prediction of curve progression in untreated idiopathic scoliosis during growth. Journal of Joint and Bone Surgery 66, pp 1061-1071.
58. Lonstein, J., Bradford, D., Winter, R., Ogilvie, J. (1995) Moe’s textbook of scoliosis and other spinal deformities, 3rd Edition. Saunders Company, Philadelphia.
59. Losito, A., Martucci, G., De Giorgi, S., Caforio, G., Caforio, L. (1996) La realización técnica del corsé Chêneau. Modelo 1994. Técnica Ortopédica Internacional, 36, pp 133-139.
60. Matthiass, H.H., Lucas, H., Benkelberg, B. (1979) Erste Versuche mit der Derotationsorthese von Chêneau. Med Orthop, 8, pp 64-72.
61. Matthiass, H.H., , J. (1984) Erste Langzeitergebnisse der Behandlung der Sloliose mit dem Cheneau-Korsett. Med Orth Techn, 69, pp104-108.
62. Mau, H. (1981) The changing concept of infantile scoliosis. Int Orthop, 5, pp 131-137.
63. McMaster, M.J. (1983) Infantile idiopathic scoliosis: can it be prevented? Journal of Bone and Joint Surgery, 65B, pp 612-617.
64. Mellencamp, D.D., Blount, W.P., Anderson, A.J. (1977) Milwaukee brace treatment of idiopathic scoliosis: late results. Clin Orthopaedics, 126, pp 47-57.
65. Miller, J.A., Nachemson, A.L., Schultz, A.B. (1984) Effectiveness of braces in mild idiopathic scoliosis. Spine, 9, pp 632-635.
66. Miller, N.H., Sponseller, E., Shugert, J., Bell, D., Schwab, N., Maestri, N. (1999) Genomic search for X-linkage in familial adolescent idiopathic scoliosis. In: Stokes (ed.),Research into Spinal Deformities 2. Studies in Health, Technology and Informatics. IOS Press, Amsterdam, pp 209-212.
67. Misol, S., Ponseti, I.V., Samaan, N., Bradbury, J.T. (1971) Growth hormone blood levels in patients with idiopathic Scoliosis. Clin Orthopaedics, 81, pp 122-125.
68. Moe, J.H. (1969) Methods and technique of evaluating idiopathic scoliosis. AAOS Symposium on the Spine, CV Mosby, St. Louis.
69. Moe, J., Kettleson, D. (1970) Idiopathic scoliosis analysis of curve patterns and preliminary results of Milwaukee brace treatment in 169 patients. Journal of Bone and Joint Surgery, 52, pp 1509-1533.
70. Nachemson, A.L. (1968) A long term follow-up study of non-treated scoliosis. Acta Orthop Scand, 39, pp 466-477.
71. Nachemson, A.L. (1996) Principles of management of idiopathic scoliosis. Proceeding of the 2nd Société Internationale de Recherche et d’Etude sur le Rachis, ( S.I.R.E.R.) meeting, Barcelona.
72. Nachemson, A.L., Peterson, L.E. (1995) Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the brace study of the Scoliosis Research Society. Journal of Joint and Bone Surgery, 77A, pp 815-822.
73. Netter, F.H. (1985) Musculoskeletal System, Part I, Anatomy, Physiology, and Metabolic Disorders. CIBA, New Jersey.
74. Nordwall, A., Willner, S. (1975) A study of skeletal age and height in girls with idiopathic scoliosis. Clinic Orthopedic, 110, pp 6-10.
75. Oberthaler, V.W., Benzer, W., Alfare, N. (1985) Boston brace versus Chêneau brace: a comparative study. Med othop Tech, 104, pp 156-161.
76. Olafsson, Y., Saraste, H., Soderlund, V., Hoffsten, M. (1995) Boston brace in the treatment of idiopathic scoliosis. Journal of Pediatric Orthopaedics, 15, pp 524-527.
77. Palastanga, N., Field, D., Soames, R. (1990) Anatomy and Human Movement.Heinemann Medical Books, Oxford.
78. Pare, A. (1634) The works of that famous Chirurgion Ambrose Parey. Translated by T. Johnson. T. Cotes and R. Young, London.
79. Pearcy, M.J. (1989) Biomechanics of the spine. Curr Orthop, 3, pp 96-100.
80. Pedriolle, R. (1979) La Scoliose. Maloine SA, Paris.
81.Peltonen, J., Poussa, M., Ylikoski, M. (1988) Three year results of bracing in scoliosis.Acta Orthop Scand, 59, pp 487-490.
82. Peterson, L., Nachemson, A.L. (1995) Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Journal of Joint and Bone Surgery, 77A, pp 823-827.
83. Reed, F.E., Price, C.T. (2002) The Charleston Bending Brace. Physician’s Manual.Charleston. pp 8-15.
84. Riddle, H.V., Roaf, R. (1975) Muscle imbalance in the causation of scoliosis. Lancet, 1,pp 1245-1247.
85. Rigo, M. (1996) Influence of physiotherapy and bracing on the deformity of the trunk in patients with idiopathic scoliosis. Proceeding of the 2nd Société Internationale de Recherche et d’Etude sur le Rachis,.S.I.R.E.R. meeting, Barcelona.
86. Rigo, M. (1997) Reconstrucción tridimensional de la columna vertebral a partir de la imagen topográfica de la superficie de la espalda. Instituto E. Salvá, Barcelona.
87. Rigo, M. (1999a) 3D correction of trunk deformity in patients with idiopathic scoliosis using a Chêneau brace. In: Stokes (ed.), Research into Spinal Deformities 2. Studies in Health, Technology and Informatics. IOS Press. Amsterdam, pp 362-365.
88. Rigo, M. (1999b) Conservative scoliosis treatment. Does the Chêneau brace change prognosis? Instituto E. Salvá, Barcelona.
89. Rigo, M. (1999c) El corsé de tipo Chêneau: Resultados preliminares. Société Internationale de Recherche et d’Etude sur le Rachis,.S.I.R.E.R, 8, pp 3-10.
90. Rigo, M. (2000) 3rd Workshop on the theory and practical aspects of the Chêneau brace. Instituto de Especialidades Ortopédicas, Sevilla.
91. Rigo, M., Chêneau, J. (1997), 2nd Orthotics Workshop on the Chêneau brace. Barcelona, Instituto E. Salvá.
92. Rigo, M., Chêneau, J. (2000), 3rd Orthotics Workshop on the Chêneau brace. Instituto E. Salva, Barcelona.
93. Rigo, M., Quera-Salvá, G., Puigdevall, N., Martínez, M. (2000) Retrospective results in immature idiopathic scoliosis patients treated with a Chêneau brace. Proceedings of the 3rd Meeting of the International Research Society of Spinal Deformities (IRSSD), Clermont-Ferrand.
94. Rigo, M., Wood, G.I. (2001a) The treatment of scoliosis with a hypercorrection TLSO- The Chêneau brace system, part 1, Barcelona.
95. Rigo, M., Wood, G.I. (2001b) The hypercorrection Chêneau brace system utilising the classification of King in the treatment of idiopathic scoliosis, part 2, Barcelona.
96. Riseborough, E.J., Wynne-Davies, R. (1973) A genetic survey of idiopathic scoliosis. Acta Orthop Scand, 50, pp 759-769.
97. Risser, J.C. (1958) The iliac apophysis: an invaluable sign in the management of scoliosis. Clin. Orthop, 11, pp 111-119.
98. Risser, J.C. (1964) Scoliosis: past and present. Journal of Joint and Bone Surgery, 46,pp 167-199.
99. Rogala, E.H., Drummond, D.S., Gurr, J. (1978) Scoliosis: Incidence and natural history, a prospective epidemiological study. Journal of Joint and Bone Surgery, 60A, pp 173-176.
100. Sahlstrand, T., Petruson, B. (1979) A study of Labyrinthine function in patients with adolescent idiopathic scoliosis. Acta Orthop Scand, 50, pp 759-769.
101. Shands, A.R., Eisberg, H.B. (1955) The incidence of scoliosis in the state of Delaware; a study of 50,000 minifilms of the chest made during a survey for tuberculosis. Journal of Joint and Bone Surgery, 37A, pp1243-1249.
102. Skogland, L.B., Miller, J.A. (1980) Growth related hormones in idiopathic scoliosis. Acta Orthop Scand, 51, pp 779-789.
103. Stokes, I.A. (1999) ‘Stress-modulated growth’ and the progression of scoliosis. In: Stokes (ed.), Research into Spinal Deformities 2. Studies in Health, Technology and Informatics.IOS Press. Amsterdam, pp 205-208.
104. Syndikus, G., Wollmer, H.W., Matthiass, H.H. (1988) Neuere Behandlungsergebnisse mit der Cheneau-Orthese im Vergleich zu Ergebnissen mit der Milwaukee-Orthese. Med Orht Tech, 108, pp 178-181.
105. Taylor, T.K.F., Phil, D., Ghosh, P., Bushell, G.R. (1981) The contribution of the intervertebral disk to the scoliotic deformity. Clinic Orthopedic, 156, pp 79-90.
106. Turner-Smith, A.R., Harris, J.D., Houghton, G.R., Jefferson, R.J. (1988) A method for analysis of back shape in scoliosis. Journal of Biomechanics, 21, pp 497-509.
107. Verbout, A.J. (1985) The development of Vertebral Column. Springer Verlag, Berlin.
108. Von Deimling, U., Wagner, U.A., Schmitt, O. (1995) Long-term effect of brace treatment on spinal decompensation in idiopathic scoliosis. A comparison of Milwaukee brace—Chêneau corset. Z Orthop Ihre Grenzgeb, 133, pp 270-273.
109. Waters, R.L., Morris, J.M. (1973) An in vitro study of normal and scoliotic interspinous ligaments. Journal of Biomechanics, 6, pp 343-348.
110. Webb, J.K., Burwell, R.G., Cole, A.A., Lieberman, I. (1995) Posterior instrumentation in scoliosis. European Spinal Journal, 4, pp 6-10.
111. Weinstein, S.L., Zavala, D.C., Ponseti. I.V. (1981) Idiopathic scoliosis. Journal of Joint and Bone Surgery, 63A, pp 702-712.
112. Weiss, H.R., Rigo, M. (1994) Chest movements during breathing in scoliosis patients, 5th Annual Meeting of the European Spine Society, Madrid.
113. Weiss, H.R., Werkmann, M. (1996) What are the quality criteria of scoliosis bracing?British Association of Prosthetists and Orthotists, 1, pp 19-25.
114. Weiss, H.R., Rigo, M., Chêneau, J. (2000) Praxis der Chêneau-Korsett versorgung in der Skoliosetherapie. Georg Thieme Verlag, Stuttgart.
115. White, A.A., Punjabi, M.M. (1978) The basic kinematics of the human spine: A review of past and current knowledge. Spine, 3, pp12-23.
116. White, A.A., Punjabi, M.M. (1990) Kinematics of the Spine. In: White A.A. and Punjabi M.M. (eds), Clinical Biomechanics of the Spine. J.B. Lippincott, Philadelphia.
117. Willner, S. (1972) Factors contributing to structural scoliosis. Thesis. University of Lund, Lund, Sweden.
118. Willner, S. (1975) A study of height, weight and menarche in girls with idiopathic structural scoliosis. Acta Orthop Scand, 46, pp 84-89.
119. Willner, S. (1982) Prospective prevalence study of scoliosis in southern Sweden. Acta Orthop Scand, 53, p 233.
120. Willers, U., Normelli, H., Aaro, S., Svenson, O., Hendlung. (1993) Long-term results of Boston brace treatment on vertebral rotation in idiopathic scoliosis. Spine, 18, pp 432-435.
121. Winter, R.B., Lovell, W.W., Moe, J.H. (1975) Excessive thoracic lordosis and loss of pulmonary function in patients with idiopathic scoliosis. Journal of Bone and Joint Surgery, 57, pp 971-977.
122. Winter, R.B., Denis, F. (1994) The King V curve pattern. Its analysis and surgical treatment. Orthop Clin North Am, 25, pp 353-362.
123 Winter, R.B., Denis, F., Lonstein, J.H., Smith, M.D. (1995) Atlas of Spine Surgery. WB Saunders, Philadelphia.
124. Wood, G.I., Rigo, M. (1999) The treatment of scoliosis with a hyper-correction TLSO- The Chêneau brace system. BAPO 5th Annual Scientific Meeting, Seminar 4, Harrogate.
125. Yamada, K., Yamamoto, H., Tamura, T. Et al. (1974) Development of scoliosis under neurological basis, particularly in relation with brainstem abnormalities. Journal of Joint and Bone Surgery, 56A, p 1764.
126. Zuk, T. (1962) Role of spinal and abdominal muscles in the pathogenesis of scoliosis. Journal of Joint and Bone Surgery, 44B, pp 102-105.
Nomenclature
1. 3-D correction: In the treatment of idiopathic scoliosis, this term refers to the correction of the deformities in all three anatomical planes. This involves correction of the coronal plane deformities (i.e.: thoracic and lumbar curves), transverse plane deformities (i.e.: pelvic torsion and thoracic rotation) and sagittal plane deformities (i.e.: hypokyphosis). The objective is that the correction occurs simultaneously in three planes of the space, as a unique movement called torsion and not plane-by-plane correction.
2. 3-curve scoliosis: Presents as one long thoracic curve with the apical vertebra around T9 to T10 or a thoracolumbar curve with the apical vertebra around T11. This long thoracic or thoracolumbar curve has two small compensatory curves, one cephalic and the other caudal.
3. 4-curve scoliosis: Presents as two main curves, one in the thoracic region and the other in the lumbar or low thoracolumbar region. These double curves have two small compensatory curves, one cephalic and the other caudal.
4. Active scoliosis brace: Refers to a scoliosis brace that applies corrective forces to physically correct the scoliotic deformity. A true active scoliosis brace must have expansion rooms to allow space for the correction of the convexities and the involuntary correction via patient respiration.
5. Adolescent idiopathic scoliosis: The most common type of idiopathic scoliosis in which appears during adolescence; at or during the pubertal growth spurt and before maturity.
6. Anteversion: An abnormal position of the hemi-pelvis that is rotated and torsioned anteriorly therefore the anterior superior iliac spine is more prominent than usual. The contralateral hemi-pelvis would be in retroversion.
7. Apical vertebra: The most rotated vertebra in a curve; the most deviated vertebra from the vertical axis of the patient.
8. Brace window: A brace window could be incorporated in most types of thermoplastic scoliosis braces. This window is an opening cut out of the plastic. Its location is usually placed on the contralateral side to the convex aspect of the coronal plane curve.
9. C1 to C7: Refers to the 1st to 7th vertebras of the cervical region. T1 to T12: Refers to the 1st to 12th vertebras of the thoracic region. L1 to L5: Refers to the 1st to 5th vertebras of the lumbar region. S1: Refers to the 1st sacral vertebra.
10. Caudal (inferior): Refers to below or towards the tail in relation to the trunk.
11. Central nervous system (CNS): The CNS is the control centre for the entire nervous system and consists of the brain and spinal cord.
Cephalic (superior): Refers to above or towards the head in relation to the trunk.
12. Charleston Bending brace: This is a custom-made thermoplastic thoracolumbosacral orthosis (TLSO) that is characterised by having a bent or curved shape and is used for part-time or night treatment of idiopathic scoliosis.
13. Chêneau brace number system: A number system is used in Chêneau brace treatment to facilitate the identification of areas and zones on the patient, positive cast and brace.
14. Cheneau brace: A thermoplastic brace modelled on a hyper-corrected positive plaster cast of the patient. It should follow the general correction principle as was written by Dubousset: “ detorsion and sagittal plane normalisation, which would effect correction of the coronal and transversal planes, resulting in some elongation of the spine, without any significant distraction force”.
15. Chêneau Toulouse-Munster (C.T.M) brace: Dr. Chêneau, inspired by Abbot, fabricated the original Chêneau brace in 1979; this brace was also called the C.T.M. (Chêneau Toulouse-Munster) brace after the French and German cities.
16. Classification of King: The classification of King distinguishes five single thoracic or combined scoliotic curve types (numbered King type I through King type V).
17. Cobb angle: This is the measurement of a scoliotic curve of the vertebral column in the coronal plane, which is measured on the coronal plane X-ray.
18. Compensatory curve: A curve, which can be structural or non-structural, above or below a major curve that tends to maintain normal body alignment. A compensatory curve is synonymous with the secondary curve.
19. Convex rib hump: Refers to thoracic vertebral rotation in which the ribs on the convex side of the coronal plane curve produce a hump or gibbus.
20. Coronal plane: A plane passing through the body from top to bottom and lying at right angles to the sagittal plane is the coronal plane. This divides the body into anterior and posterior parts.
21. Corrective pads: Some scoliosis braces have corrective Pelite pads, which are used for the correction of the curves in the coronal and transversal planes and therefore are placed on the convex side of the curve.
22. CTLSO: A cervicothoracolumbosacral orthosis.
23. Derotate: Correction of the rotational aspect of the vertebral column.
24 Detorsion: Correction of the torsional aspect of the vertebral column.
25. Discs degeneration: Refers to the degeneration of the intervertebral discs in the vertebral column.
26. Dorsal (posterior): Refers to the rear or behind.
27. Dynamic scoliosis brace: A scoliosis brace that dynamically changes the transmitted loads to the curves, simultaneously with the scoliosis correction. This could be achieved by elastic pads or bands, as applied in the Spine Cor system.
28. Electromyography (EMG): The evaluation of electrical activity in resting and contracting muscles.
29. End vertebra (upper and lower): Upper, the most cephalic vertebra of a curve, whose superior surface tilts maximally toward the concavity of the curve. Lower, the most caudal vertebra whose inferior surface tilts maximally toward the concavity of the curve.
30. Expansion room: The scoliosis brace and positive plaster cast have expansion room (also called chamber, space, area and zone) built in to provide room or space for the correction of the scoliotic deformity. Expansion rooms on the positive cast are made by adding plaster in the required area therefore producing a space when the negative brace is fabricated. Expansion rooms are produced in the scoliosis brace by the aforementioned way and/or by physically cutting out the brace, which provides a window for the expansion of the deformity.
31. Flat back effect: This effect is produced by the majority of TLSO braces, in which the design of the brace produces flat back or hypokyphosis.
32. Flat back: Refers to the abnormal physical appearance “flat” of the back surface in the sagittal plane of the thoracic region, also called hypokyphosis.
33. Formetric System: Provides a method to measure the back surface of the subjects’ trunk. The Formetric system reconstructs and automatically analyses back shape, based on the video-stereograph reticular which projects lines over the patients´ back.
34. Geometrical or helicoidal torsion: Refers to the twisting of the spine, which is considered as a line in space. Thevertebral column, moved by deforming forces, changes its physiological shape in the coronal, transversal and sagittal planes, adopting extremely diverse anatomoradiological patterns.
35. Global coronal plane: Frontal plane in the global coordinate system.
36. Hidden King type IV and hidden King type V: A significant number of scolioses patterns that have the criteria to be diagnosed as a King type III, are actually King type IV patterns or King type V patterns or both. As a result of the difficultly in the diagnosis of the classification of the curve pattern, they are referred to as hidden King type IV or hidden King type V.
37. Hyper-corrected positive-cast: Refers to the modified positive cast of a Chêneau brace in which aggressively rectified pressure points and expansion rooms can be clearly observed.
38. Hyperkyphosis: A sagittal alignment of the thoracic spine in which there is more than the normal amount of kyphosis (a kyphos).
39. Hypokyphosis: A sagittal alignment of the thoracic spine in which there is less than the normal amount of kyphosis, but it is not so severe to be truly lordotic.
Idiopathic scoliosis: A structural spinal curvature of the coronal plane in an otherwise healthy child, for which no cause is established.
40. Iliac rotation: Refers to a situation of relative retroversion of the convex side of the lumbar curve and anteversion of the concave lumbar side.
41. Infantile idiopathic scoliosis: Idiopathic scoliosis in which has its onset before three years of age.
42. Intervertebral torsion: Torsion that occurs in the intervertebral disc, which produces a change in the orientation of the transversal plane between two vertebras of the spine.
43. Intrapelvic rotation: Refers to a true bone deformity, which is present in the pelvis.
— Juvenile idiopathic scoliosis: Idiopathic scoliosis appearing between the ages of three and the beginning of adolescence (onset of puberty).
44. Kyphosis: This term is used to describe the normal physiological sagittal plane (posterior-arch) of the thoracic and sacral regions of the vertebral column. The normal range of kyphosis in children is between 20 to 40 degrees on sagittal plane X-ray evaluation.
45. Large diameter: This refers to the larger than normal diameter of the thorax in the transverse plane; which is caused by the hypokyphosis of the sagittal plane.
— Lateral deviation: This topography value is the measurement of the coronal plane deformity using the Formetric system.
46. Lateral Shift: This term is used in the treatment of scoliosis when using the Charleston Bending brace. It refers to a 3-point pressure which is applied to the apex of the major curve. The stabilising and unbending forces work with the lateral shift.
47. Lateral: Refers to away from the median plane or midline.
48. Lordosis: This term is used to describe the normal physiological sagittal plane (anterior-arch) of the cervical and lumbar regions of the vertebral column. Scoliosis braces endeavour to obtain normal physiological lordosis by incorporating 20 to 25 degrees of lumbar lordosis into the brace.
49. LSO (Boston) brace: A thermoplastic scoliosis brace used to treat the coronal plane curve and transversal rotation of the lumbar and sacral regions of the vertebral column. This brace is made from a prefabricated module or made-to-measure cast.
50. LSO: A lumbosacral orthosis.
51. Lumbar plate: This is a corrective plate used in scoliosis braces (i.e. Lyon brace), which is adapted to the convex side of the lumbar curve in the coronal plane.
— Lumbosacral fossas: An anatomical reference that is characterised by two dimples on the posterior side of the pelvis and are located at the posterior superior iliac spines.
52. Made-to-measure: These are custom-made braces that are fabricated from a positive cast of the patients’ trunk. Subsequently the negative cast is rectified to the requirements of the brace type.
53. Major curve: Term used to designate the largest structural curve.
54. Mechanical torsion: Refers to the torsional deformity of the vertebral column, which the spinal column is considered as a plastic structure, this includes an intravertebral torsion and an intervertebral torsion.
55. Medial: Refers to towards the median plane or midline.
56. Milwaukee brace: A CTLSO scoliosis brace used to treat the coronal plane curve of the cervical, thoracic, lumbar and sacral regions of the vertebral column. It consists of a contoured pelvic girdle attached by three uprights to an occipital pad and throat mould of the chin piece.
57. Minor curve: Term used to refer to the smallest curve, which is always more flexible than the major curve.
58. Multifactorial: A condition that is caused by multiple factors.
59. Non-progressive curve or non-progressive scoliosis: A scoliotic curve, in which the Cobb angle does not increase 5 degrees or more during a six-month period.
60. Non-structural curve: A curve that has no structural component and that corrects or overcorrects on recumbent side-bending roentgenograms. A non-structural curve has normal flexibility.
61. Oval oblique thorax: In a transverse section of the thorax in which hypokyphosis is presented, the thorax has an oval shape that is oblique to the transverse plane. Therefore the diameter of the thorax is larger than normal due to the hypokyphosis of the sagittal plane.
62. Paraspinal zone: This refers to the area on the positive cast in which a vertical axis is drawn caudally from the centre of the pelvis, with the lumbosacral fossas as the anatomical reference. This term has been introduced by Rigo in order to give clear rules in the positive cast modification.
63. Passive correction brace: A scoliosis brace that does not have space or windows for active correction of the spine. Correction is passive with the spine being pushed into the corrected position and then being held there by the tight fitting brace without the need for active muscular effort.
64. Pedriolle method: Pedriolle method of measurement of vertebral rotation using a torsiometer which is superimposed on the vertebra. The measurement is made from the pedicle situated at the convexity of the apical vertebra under consideration.
65. Pelvic obliquity: Deviation of the pelvis from the horizontal in the coronal plane. Fixed pelvic obliquities can be attributable to contractures either above or below the pelvis.
66. Pelvic section: This is the section of a scoliosis brace that covers the pelvis and plays an important roll in the suspension on the brace via the pelvic grip of the waist.
67. Postural equilibrium dysfunction: A disorder that produces an imbalance of posture.
68. Prefabricated module: These are prefabricated braces (i.e.: Boston brace system) that come in various sizes, which are fit and adapted to the patient for treatment of scoliosis.
69. Pressure points: The scoliosis brace and positive plaster cast have pressure points built-in to force the scoliotic deformity in a way that corrects the deformity by a physical force. Pressure points or areas on a positive cast are made by taking off plaster in the required area therefore producing pressure when the negative brace is fabricated. Pressure points are produced via the scoliosis brace by the aforementioned way or by Pelite pads.
70. Primary curve: This is the first or earliest of several curves to appear, if identifiable. Also, called a main and major curve.
71. Progressive curve or progressive scoliosis: A scoliotic curve, in which the Cobb angle increases 5 degrees or more during a six-month period. Progression is also considered to be a sustained increase in the Cobb angle of at least 10 degrees.
72. Re-kyphosis: Correction of the hypokyphosis by returning the vertebral column in the thoracic region the normal physiological kyphosis of the sagittal plane.
73. Retroversion: An abnormal position of the hemi-pelvis, which is rotated and torsioned posteriorly therefore the anterior superior iliac spine is less prominent than usual. The contralateral hemi-pelvis would be in anteversion.
74. Rigo Model: The Chêneau brace (Rigo Model) refers to the treatment of scoliosis using the Chêneau brace and the classification of King to prescribe the brace model and its characteristics for each individual case.
75. Risser sign: Patient maturity is measured by the ossification of the iliac epiphysis. Ossification normally starts at the anterior superior iliac spine (ASIS) and progresses posteriorly to the posterior superior iliac spine (PSIS). Risser divided the excursion into four quarters, Risser sign 1 through 4, with Risser sign 5 once complete ossification has occurred and fusion to the iliac crest takes place.
76. Rotation: This topography value is determined by measurement of surface rotation. The surface rotation is measured by the normal surface angle at the level of the spinous processes.
77. Sagittal normalisation: The correction of the hypokyphosis in thoracic region of the vertebral column. Sagittal normalisation is achieved by obtaining a normal physiological kyphotic curve in the thoracic region.
78. Sagittal plane: Passing through the body from front to back and dividing it into two symmetrical right and left halves. Any plane parallel to this is known as a sagittal plane.
79. Stabilising force: This term is used in the treatment of scoliosis when using the Charleston Bending brace. It refers to a 3-point pressure which is applied to the hemipelvis or lower lumbar region on the opposite side to the lateral shift.
80. Structural curve: A segment of the spine with a lateral curvature that lacks normal flexibility. Radiographically, it is identified by the complete lack of a curve on a supine film or by the failure to demonstrate complete segmental mobility on supine side-bending films.
81. Thoracic plate: This is a corrective plate used in scoliosis braces (i.e. Lyon brace), which is adapted to the convex side of the thoracic curve in the coronal plane.
82. Three-dimensional (3D): This term when used in scoliosis, refers to the three anatomical planes, coronal, sagittal and transversal planes.
83. Three-point pressure system: These are 3 forces applied to a curve or deformity for correction. This is achieved by one force applied in the centre of the convex side of a curve, with two counter forces applied to the each end of the contralateral side of the curve.
84. TLSO (Boston) brace: A thermoplastic scoliosis brace used to treat the coronal plane curve and transversal rotation of the thoracic, lumbar and sacral regions of the vertebral column. This brace is made from a prefabricated module or it is made-to-measure.
85. TLSO: A thoracolumbosacral orthosis.
86. Topography value: The measurement of the patients´ back surface with the Formetric system provides the three following topography values: lateral deviation, rotation and trunk length.
87. Torsion angle: This is the measurement of the scoliotic curve rotation of the vertebral column in the transversal plane, which is measured on the coronal plane X-ray using the Pedriolle’s torsiometer.
88. Transversal deformity: Scoliosis often produces transversal deformities in which the shoulders and greater trochanters are deviated away from the midline of the body in the coronal plane, therefore producing an unbalanced coronal plane. This deformity is corrected by aligning the midpoint of the occiput over the sacrum in the same vertical plane as the shoulders are relative to the hips.
89. Transverse plane: A plane passing through the body at right angles to both the sagittal and coronal planes dividing it into upper and lower parts is known as the transverse plane.
90. Trunk length: This topography value is the measurement of the subjects’ trunk length. The trunk length is determined by measuring the distance from the posterior iliac fossa to the 7th cervical vertebra.
91. Unbalanced coronal plane: This is produced by a transversal deformity in which the trunk and shoulders are deviated away from the midline of the pelvis.
92. Ventral (anterior): Refers to the front or in front.
93. Unbending force: This term is used in the treatment of scoliosis when using the Charleston Bending brace. It refers to a 3-point pressure which is applied to the axillar region on the opposite side to the lateral shift.
94. Viscoelastic linkages: Refers to the vertebra as individual links, which are connected by viscoelastic materials such as intervertebral discs and ligaments.
95. Wilmington brace: This is a custom-made underarm jacket or brace (LSO) fabricated in thermoplastic, used for part-time or night treatment of idiopathic scoliosis.